Advancements in organoid technology have led to novel stem cell–based models that reflect important structural and functional properties of the tissue from which the cells were derived in vivo. These models provide more clinically relevant platforms that can help researchers better select agents to advance to the clinic.
This blog post explores key differences between organoid types and why adult stem cell (ASC)-derived in vitro organoids are superior patient-relevant 3D models.
The Definition of Organoids
Historically, “organoid” has been used rather loosely, mostly referring to aggregates of cells that form 3D structures when cultured without attachment substrates.
However, it now generally describes a 3D structure that has
- Cells that establish or retain the identity of the organ/tissue being modeled (both stem cells and their progeny),
- Multiple cell types found in the original organ/tissue,
- Some aspect of the specialized function of the original organ/tissue, and
- Self-organization that parallels the same intrinsic organizing principles as those in the original organ/tissue.
How Organoids Differ from Spheroids
3D organoids, which can be derived from both healthy and diseased tissues (e.g., tumor organoids) differ from other 3D models. For instance, spheroids from tumor cells—also referred to as “tumorspheres”—are established from a single cell type or a multicellular mixture and can originate from stem cells, primary cells, immortalized cell lines, or human tissue.
Tumorspheres are cultured in conditions that select them to have a high proportion of poorly differentiated cells with high replicative potential (i.e., primarily cancer stem cells [CSCs]).
They typically contain layers of cells. Some are exposed to the surface and others buried within the sphere. As a result, spheroids are very heterogenous and can include oxygenated or hypoxic cells that are proliferating, nonproliferating, or necrotic.
Long-term culturing of patient-derived tumorspheres also remains a challenge. This may be due to inherent technical difficulties in extracting and maintaining viable cells. For instance, data suggest that such tumorspheres only briefly retain the important properties of the original tumor.
In comparison, organoids are typically derived from either:
- pluripotent stem cells (PSCs) (i.e., embryonic stem cells or induced pluripotent stem cells [iPSCs]) or;
- multipotent organ-specific adult stem cells (ASCs).
They can be composed exclusively of either epithelial cells or a mixture of epithelial and mesenchymal cells. The choice of starting material leads to important differences in the organoids and their applications, including for oncology research and drug development.
Main Differences Between PSC- and ASC-Derived Organoid Development
PSC-derived organoids are typically used to model organogenesis because the PSCs differentiate from premature tissues into near-native organotypic cultures. Compared to ASC-derived organoids, an additional step is required to drive the differentiation toward the germ layer that yields the desired organoids (endo-, ecto-, and mesoderm).
This is done by supplementing the cell culture medium with specific growth factors. For iPSCs, somatic stem cells are differentiated into PSCs and genetically reprogrammed toward an endo-, ecto-, or mesoderm fate.
In contrast, ASC-derived organoids are established from tissue-specific stem cell populations using optimized protocols. These enable purified single ASCs or tissue-specific microstructures to serve as the source material.
Culture conditions are optimized to preserve the stem cells’ self-renewing and differentiating potential, supplementing key tissue-specific stem cell niche factors, and using Matrigel as a surrogate for the extracellular matrix.
This is a faster approach because ASCs do not require reprogramming to differentiate into the appropriate lineage. Omitting a mesenchymal niche also helps generate more robust models because mesenchymal cells can affect culture stability.
ASC organoids are quicker to establish because they do not require extra genetic reprogramming and differentiation steps. They are more easily scalable, highly stable in vitro over the long term, and proven to be patient-relevant and clinically predictive.
As protocols have continued to advance, organoid development has become increasingly possible for large array of normal and diseased tissues, including many types of solid cancers.
ASC Organoids: The Only Clinically Relevant Organoid Models
While PSCs can be genetically engineered to introduce oncogenic or tumor suppressor mutations, these processes produce tumor-like growths but lack the complexity of the genetic makeup of each clinical tumor. This can only be recapitulated by starting with patient material and is a major reason that ASC tumor organoids are the most clinically relevant models available for oncology drug development.
Data from many publications (for example, here, here and here) have established adult stem cell derived tumor organoids as the most clinically relevant 3D in vitro models to show the following:
- Genomic and phenotypic stability in long-term culture and after cryopreservation,
- Enhanced clinical predictivity, and
- Ease of scalability relative to in vivo models.
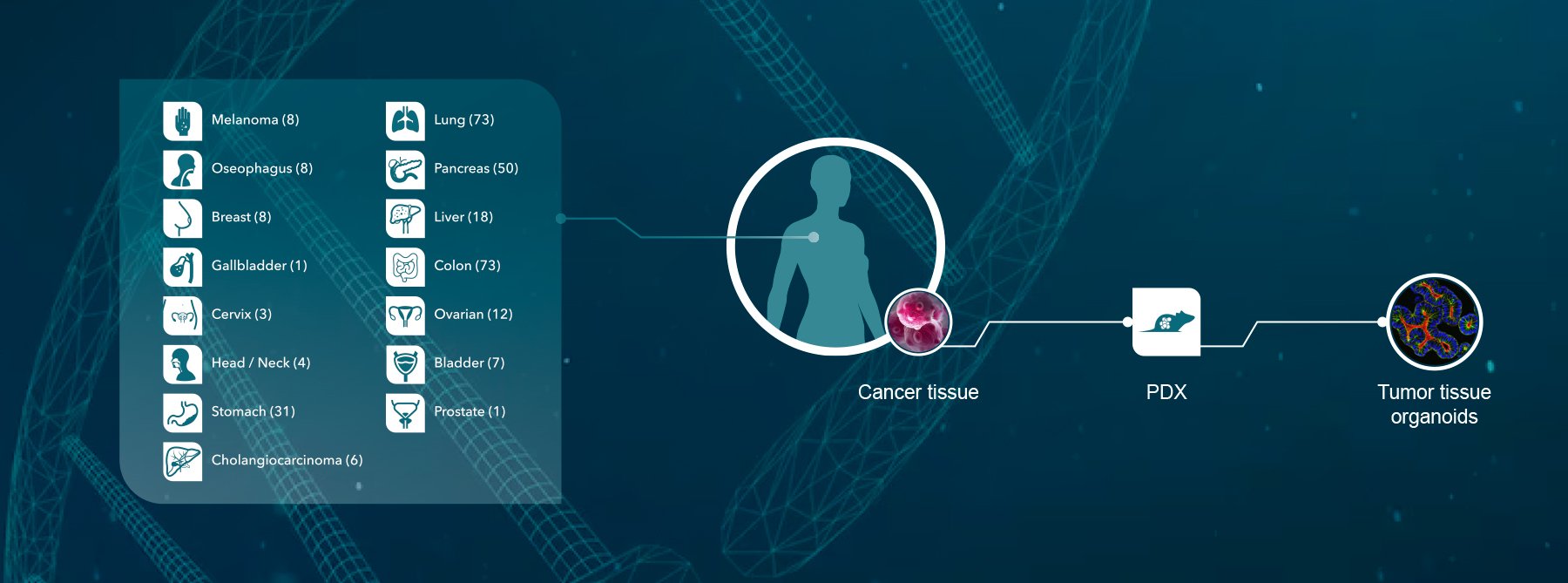
3D in vitro organoids have been developed from a wide variety of primary human tumors that preserve the CSC component. Tumor organoids are primarily epithelial in origin, and they can be produced from a wide spectrum of cancer types using tissue directly from patient tumors (patient-derived organoids) or patient tumor tissue expanded in mice as PDXs (PDX-derived organoids).
Both types have been shown to faithfully recapitulate the complexities of human cancer tissue, including CSCs and their differentiated progeny.
Tumor Organoids Can Accelerate Oncology Drug Development
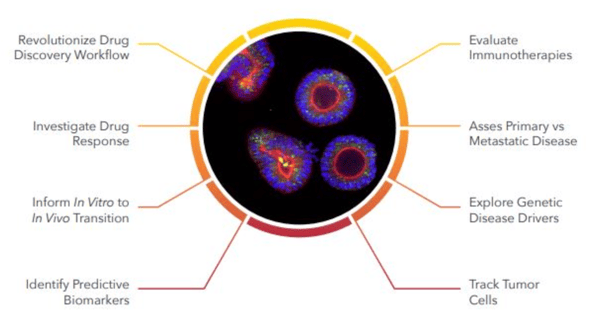
Tumor organoids have emerged as powerful predictive preclinical models for cancer drug discovery and development. Given their unique attributes, their value has been increased by developing biobanks (with matched healthy tissue) that capture phenotypic and genetic patient-population heterogeneity, support large-scale studies, and ensure availability for repeat studies.
These large “living” tumor organoid biobanks allow you to bring “patients to the lab” and can be used to conduct large-scale population studies investigating treatment response and to identify biomarkers. This approach is the equivalent of a clinical trial but carried out in a dish. It expedites drug development and reduces the high attrition rate of oncology candidates.
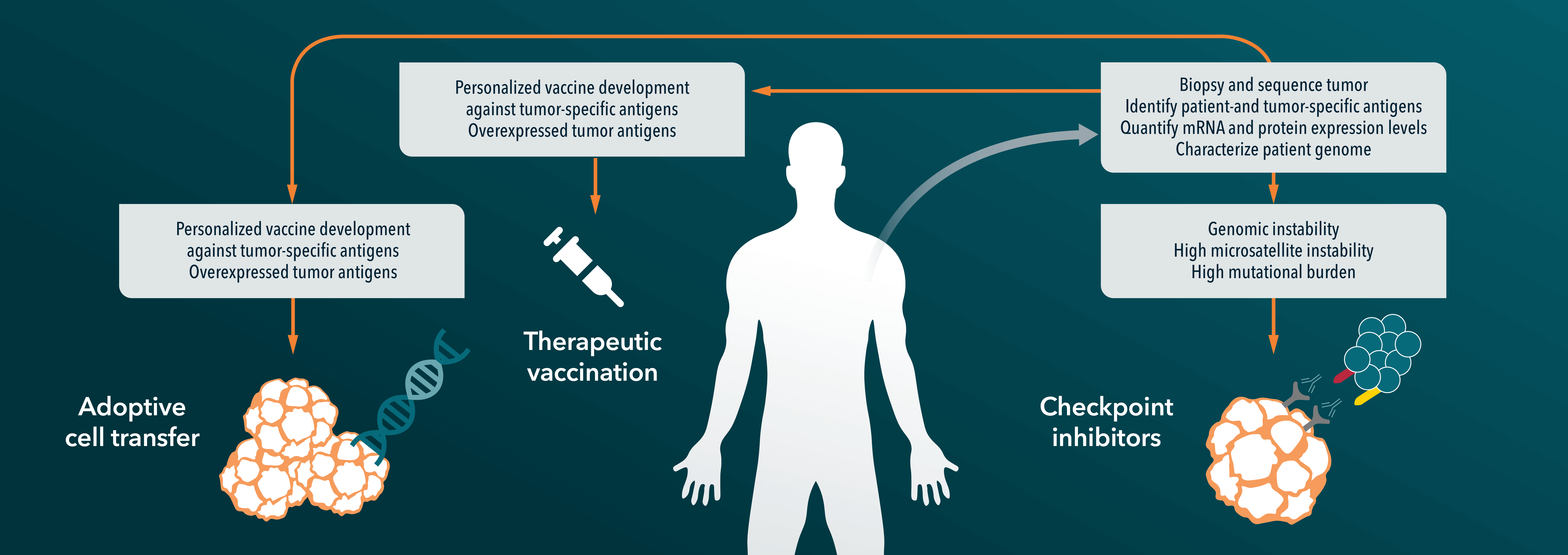
Tumor organoid co-cultures are also being used for I/O applications. This offers another preclinical platform that is more clinically relevant compared to cancer cell lines and can be used to test novel immunotherapies in vitro using co-cultures of tumor organoids with various human immune cell types, including TILs, CAR-T, or specific tumor microenvironment components. Such studies can provide key insights that lead to an antitumor response and enable drug screens that test the efficacy of novel immunotherapies and drug combinations.
Conclusion
Organoids can be produced using different types of stem cells (PSCs and ASCs). However, only specialized protocols have been demonstrated to produce clinically relevant tumor organoids that can accelerate cancer drug development.
Watch our on-demand webinar, where we interview Michiel Fokkelman, the head of high throughput screening at Crown Bioscience. Michiel is a seasoned expert in the field of high content imaging, he shares his wealth of knowledge and insights on this critical area of research. In this episode, you will learn all about the latest developments in high content imaging and how it is revolutionizing drug discovery and pre-clinical drug development.