In this blog article we explore what we have learned about the genetics of hematological cancers, and how it can be modeled for research and drug discovery.
How Does Hematological Cancer Develop?
Hematopoiesis is a dynamic developmental process, arising from hematopoietic stem cells (HSCs) in the bone marrow to maintain the lifelong regeneration of blood cells. Perturbation of normal hematopoietic differentiation results in hematological cancers. These are subdivided into three main types: multiple myeloma, leukemia, and lymphoma.
This post reviews the differences in genetic abnormalities across the range of hematologic malignancies, the variety of targeted agents developed, and the preclinical models used to assess potential new therapeutics.

Multiple Myeloma (MM)
Multiple myeloma affects the plasma cells within the bone marrow that are responsible for the production of antibodies. Plasma cells accumulate in the marrow, and damage or weaken the bone, inducing bone pain. Cancerous plasma cells can also produce abnormal antibodies which alter the humoral immune response, increasing the risk of infection and the ability to combat infection.
MM initiation and progression is due to genetic alterations and chromosomal abnormalities, including translocations, duplications and insertions. The most commonly reported genetic changes involved MEK/ERK signaling (KRAS, NRAS, BRAF, NF1, PTPN11 FGFR3); G1/S perturbation (TP53, RB1 CDKN2C, CCND1); RNA processing (FAM46C, DIS3); and epigenetic regulators (DNMT3A, TET2 and KDM6A). These genetic changes play a role in the pathogenesis of MM, providing prognostic and therapeutic targets for novel therapies.
Over the past decade, treatment options for multiple myeloma have increased substantially, including:
- Chemotherapies
- Corticosteroids
- Immunomodulating agents (thalidomide, lenalidomide, pomalidomide)
- Proteasome inhibitors (bortezomib, carfilzomib, ixazomib)
- HDAC inhibitors (panobinostat)
- Monoclonal antibodies (daratumumab, elotuzumab)
- Chimeric antigen receptor T cells
- T cell–engaging bispecific antibodies
- Antibody–drug conjugates
Leukemia
Leukemia is caused by excessive production of abnormal white blood cells in bone marrow, which then circulate into the blood. Leukemia can be categorized into multiple subtypes: acute lymphocytic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL), and chronic myeloid leukemia (CML). Acute leukemias are fast-growing and may require aggressive treatments.
Acute Lymphocytic Leukemia (ALL)
Although ALL is a heterogenous group the primary genetic lesions that cause the vast majority of ALL are still unknown, a high frequency of genetic abnormalities are observed. In B-ALL this includes:
- Translocations (such as ETV6/RUNX1, BCR/ABL1, TCF3/PBX1)
- MLL rearrangement involving 11q23 with a wide range of partner genes
- Rearrangement of MYC into antigen receptor gene loci
- Mutations of genes involved in tumorigenesis or tumor suppression, apoptosis, and cell cycle regulation (e.g. CRLF2, IKZF1, TP53, and FLT3)
- In T cell ALL, LYL1, TAL1, TLX1, and TLX3 rearrangements occur.
The main treatment for ALL in adults is typically long-term combination chemotherapy. This incorporates tyrosine kinase inhibitor targeted therapy (e.g., imatinib, dasatinib, nilotinib, ponatinib, bosutinib) for patients harboring BCR-ABL rearrangement.
Immunotherapies are also used as second line treatment for refractory or relapsed ALL. This includes blinatumomab a bispecific T cell engager targeting CD19, the monoclonal antibody inotuzumab ozogamicin (Besponsa®) against CD22, or the CAR-T cell therapy tisagenlecleucel (Kymriah®) targeting CD19. Radiation therapy and stem cell/bone marrow transplants can be also used in certain situations.
Acute Myeloid Leukemia (AML)
AML is a heterogeneous disease whose onset involves a variety of chromosomal abnormalities and gene mutations. The most important of these gene mutations for differentiated prognosis are the internal tandem duplication (FLT3-ITD), NPM1, IDH1, IDH2, and CEBPA gene mutations.
The main treatment for most types of AML is chemotherapy, commonly using cytarabine or anthracycline drugs. Sometimes targeted therapies are used in combination with chemotherapy, such as adding FLT3 inhibitors (midostaurin, gilteritinib, quizartinib) or IDH inhibitors (ivosidenib, enasidenib). Gemtuzumab ozogamicin (GO) is an immunotherapeutic agent is used to treat newly diagnosed CD33 positive patients.
Chronic Lymphocytic Leukemia (CLL)
In CLL, TP53 is the most clinically adverse mutation, with less frequent mutations observed in NOTCH1, SF3B1, PO1, EGR2, MYD88, the WNT pathway, and deletion 11q-associated mutations (ATM, BIRC3). Mutations in BTK and PLCG2 are also found in approximately 80% of CLL patients with acquired resistance to ibrutinib.
CLL is treated by a variety of different drug types, such as:
- Chemotherapy
- Radiation therapy
- Monoclonal antibodies targeting CD20 (rituximab, obinutuzumab, ofatumumab)
- mAb targeting CD52 (alemtuzumab)
- mAb targeting CD22 (Lumoxiti™)
- BTK inhibitors (ibrutinib, acalabrutinib, zanubrutinib)
- BTK degraders (NX-2127)
- PI3K inhibitors (idelalisib, duvelisib)
- Bcl-2 inhibitors (venetoclax)
- Autologous stem cell transplantation
- The CAR T cell therapy lisocatagene maraleucel (Breyanzi®) is used to treat therapy-resistant CLL
Chronic Myeloid Leukemia (CML)
The primary cause of CML is BCR-ABL gene rearrangement. Additional chromosomal changes and mutations in tumor suppressor genes and oncogenes (e.g., p53, Rb1, or RAS), are required for the progression from chronic to acute leukemia.
As CML patients harbor BCR-ABL rearrangement, targeted therapy using tyrosine kinase inhibitors (imatinib, dasatinib, nilotinib, ponatinib, bosutinib) is the standard treatment. Chemotherapy or interferon therapies are also used. Asciminib is used for chronic CML patients who have failed two lines of therapy and carry the T313I mutation.
Lymphoma
Around half of the hematologic cancers that occur each year are lymphomas, or cancers of the lymphatic system. Lymphomas develop from lymphocytes (T or B cells) that expand out of control. They circulate through the blood and lymphatic system to reach and grow in many parts of the body, including the lymph nodes, spleen, bone marrow, and other organs.
There are dozens of types of lymphoma. The two main categories are Hodgkin's lymphomas (HL); and non-Hodgkin lymphomas (NHL) which account for approximately 90% of disease.
HL is marked by the presence of Reed-Sternberg cells, which are mature B cells that have become malignant. By contrast, NHL is derived from B cells or T cells, and can arise in the lymph nodes as well as other organs.
Prognoses and treatments are different for HL, and also differ between the many forms of NHL. In HL, in addition to chemotherapy or radiotherapy, immunotherapy is used, such as monoclonal antibody anti-CD30 (brentuximab vedotin), anti-CD20 (rituximab) or immune checkpoint inhibitors targeting anti-PD1 (nivolumab, pembrolizumab).
NHL has some overlap in the treatments that are used. In addition to chemotherapy or radiotherapy, immunotherapies which are approved include:
- Monoclonal antibody anti-CD30 (brentuximab vedotin)
- mAb anti-CD20 (rituximab, obinutuzumab, ofatumumab, ibritumomab tiuxetan)
- mAb anti-CD52 (alemtuzumab)
- Immune checkpoint inhibitor anti-PD1 (nivolumab, pembrolizumab)
- Immunomodulating drugs (thalidomide, lenalidomide)
- CD19 CAR-T therapy (axicabtagene ciloleucel, tisagenlecleucel)
Preclinical Models for Testing Hematologic Cancer Agents
Translational preclinical models are needed to help to better understand the complex biology of hematologic cancers and to evaluate potential new or combination therapies.
Models of hematologic malignancies have traditionally been cell line derived xenograft models, using cell lines which have been immortalized from patient tissues in vitro.
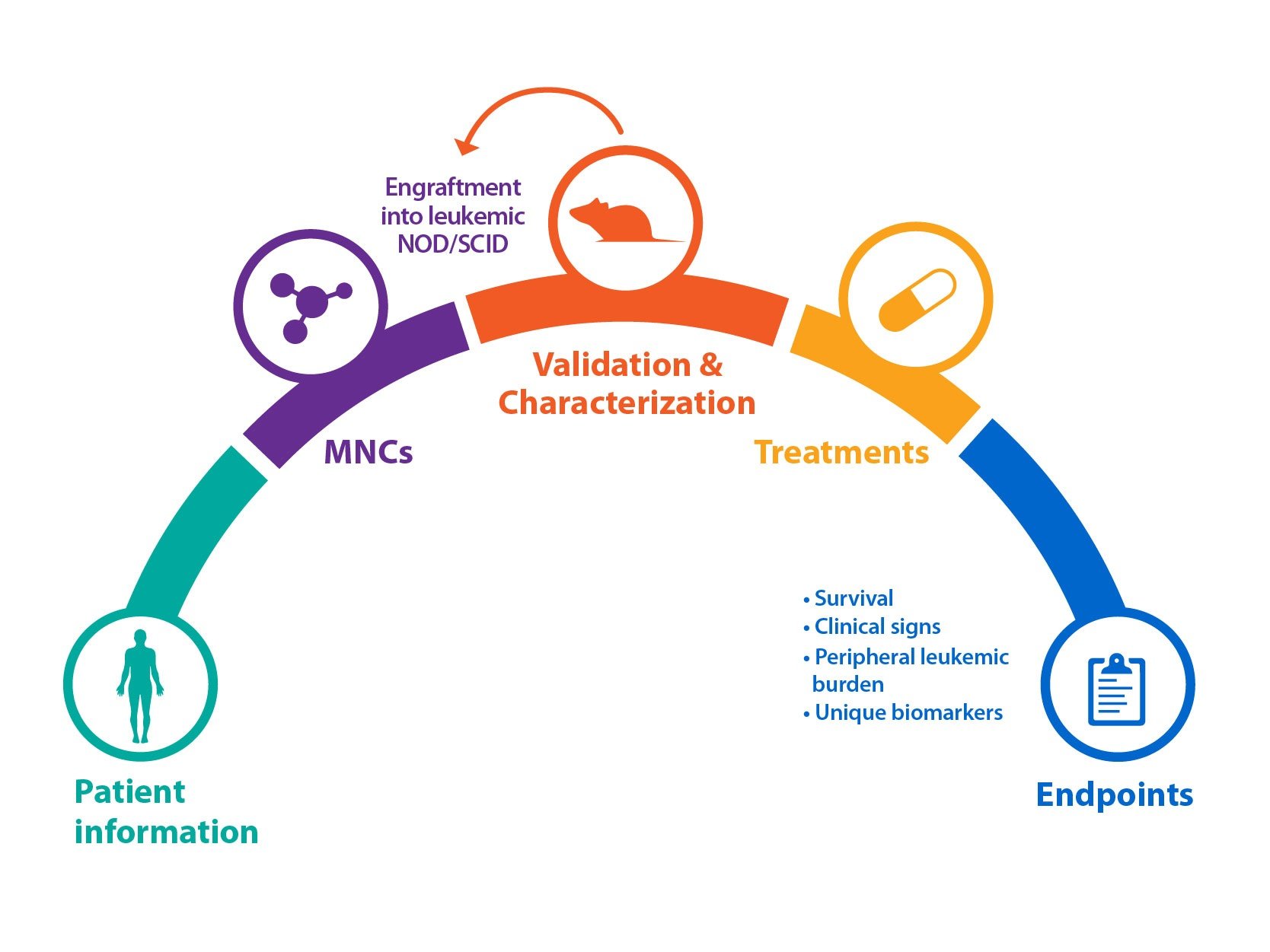
Crown Bioscience's PDX Platform
Highly predictive patient-derived xenograft (PDX) preclinical models have also been developed from a patient’s blood, which are implanted directly into mice without in vitro propagation. To develop these models, peripheral blood or bone marrow is taken from patients, and implanted into mice to generate the original model. This model is utilized to evaluate lead compounds for a variety of pharmacological properties (PD, efficacy, etc.), as well as disease indication and demographic specificity.
Despite the challenges in developing those models, a significant number of models are now available depending on the indication and subtype. For instance, a variety of AML phenotypes are now represented. This includes models which are not very differentiated and mostly limited to the bone marrow, and PDX which show more differentiated disease, moving into peripheral organs and with features such as enlarged spleens. PDX models represent genetically defined subgroups for many indications. These models accurately can specifically evaluate therapies that target ‘druggable’ mutations.
As PDX models closely reflect patient tumor histo- and molecular pathology they offer a highly predictive model for preclinical drug evaluation for hematologic cancer.
Conclusion
The wide variety of hematologic cancer genotypes and phenotypes means that a raft of targeted agents, immunotherapies, and combination regimens are needed to combat the disease. Preclinical models are needed which capture clinical disease diversity, and PDX models offer a powerful and predictive option when assessing the next generation of hematologic cancer agents.