 “Cancer progression” is the process by which this disease goes from bad to worse. Molecularly, the course of cancer progression is set by accumulation of mutations in genes, resulting in activation and inactivation of oncogenes and suppressor genes. At the cellular and tissue level, advanced cancers evade the immune system, stimulate the development of a blood supply, invade surrounding tissues, and metastasize.
“Cancer progression” is the process by which this disease goes from bad to worse. Molecularly, the course of cancer progression is set by accumulation of mutations in genes, resulting in activation and inactivation of oncogenes and suppressor genes. At the cellular and tissue level, advanced cancers evade the immune system, stimulate the development of a blood supply, invade surrounding tissues, and metastasize.
This last feature, the sinister spread of cancer cells throughout the body, is responsible for cancer mortality. Yet, in most presentations, a deep study of cancer progression has proven difficult.
Cancer Progression is Difficult to Study
Why is this? Most cancers develop in tissues which are not easily observed or monitored. We only notice cancer when it becomes symptomatic, which is typically characteristic of late-stage disease. Early-stage, non-symptomatic lesions are elusive, so an appreciation for the molecular and cellular events that conspire to make a cancer progress are less well understood. There is one notable exception – melanoma.
Using Melanoma to Study Cancer Progression
As melanoma lesions develop on the skin surface, they are easily detected and removed. With adequate screening, melanoma could easily move from our medical textbooks and into medical history. For now, the cutaneous presentation of melanoma supports comparative study of early-stage and late-stage lesions, given us a temporal view of cancer progression.
Tissue Microanatomy
To provide context, it is important to review some tissue micro-anatomy. Generally, tissues are divided into two main compartments:
- the parenchyma is the part of any tissue that performs its function
- while the mesenchyme or stroma is the part of the tissue that supports the parenchyma.
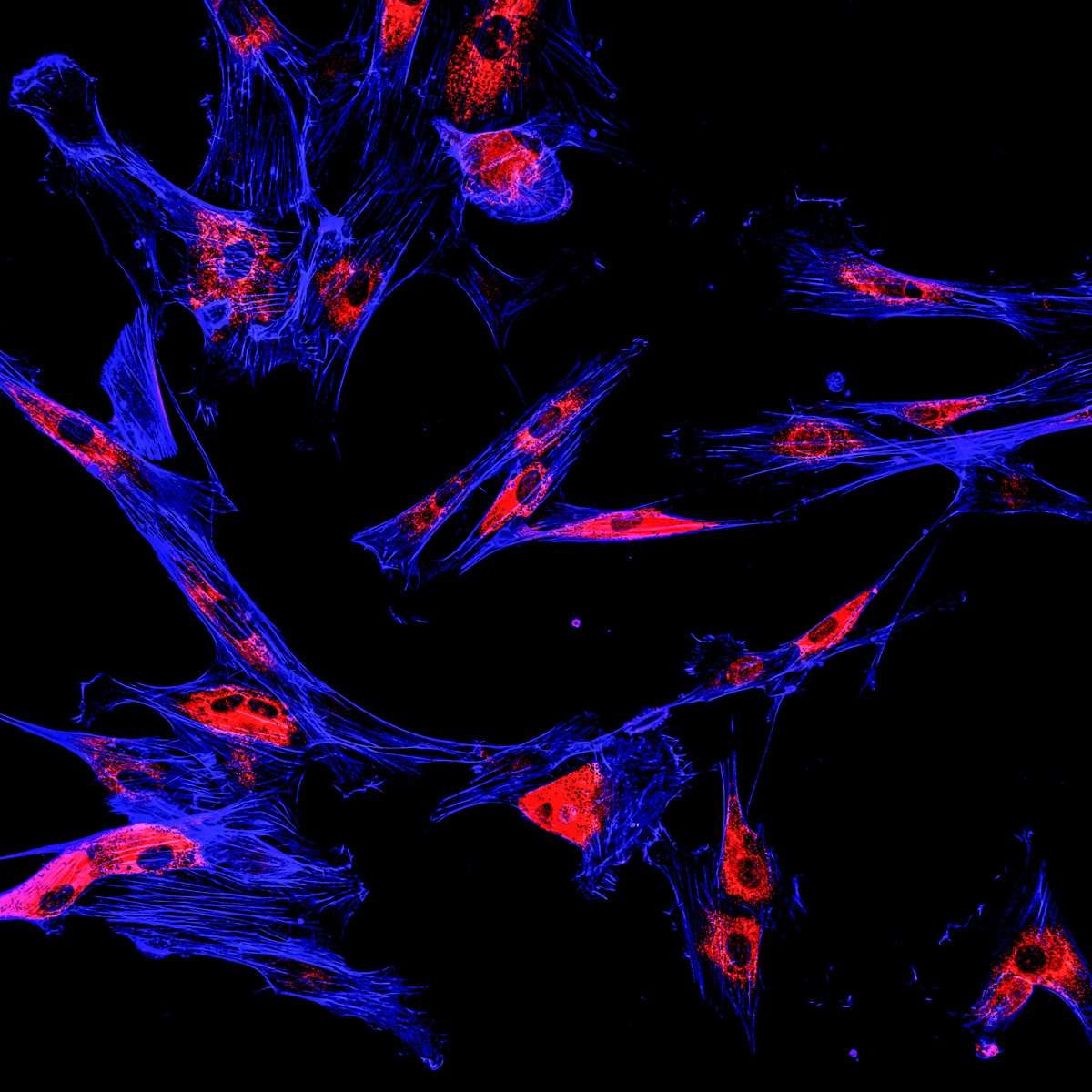
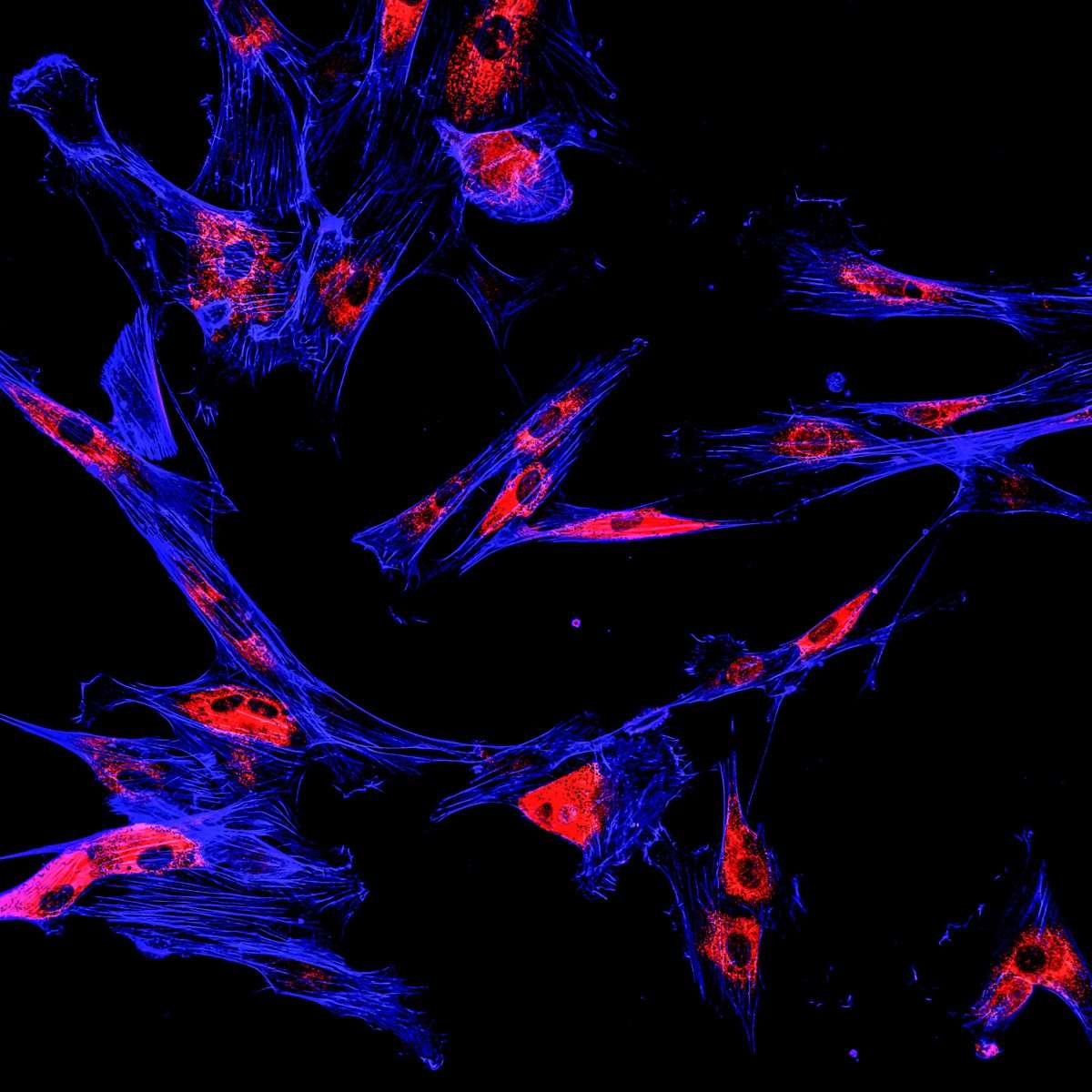
In a true epithelium, like the skin, the parenchyma and mesenchyme are separated by the basement membrane, a thin type IV collagen-containing layer like the frosting between layers of a cake. The precursor cells to melanoma, melanocytes, reside in the epidermis, which is the parenchymal compartment of the skin. The dermal layer of the skin is the mesenchymal compartment, where the supporting stromal cells reside.
Understanding Why Melanoma Metastasizes
In the histopathological classification of melanoma, it was thought that the thickness of a lesion was a key feature to predicting the outcome for a patient. While prognostication based on lesion thickness generally held true, too frequently were there instances of thick lesions that were non-life threatening. More importantly, too frequently were there instances of thin lesions that were fatal (i.e. metastatic). Something was missing.
Wallace Clark Jr., a pathologist at Mass General Hospital, developed a compelling hypothesis regarding thin but metastatic melanomas. A common feature of these thin metastatic melanomas was that they were present in the dermis of the skin, having invaded through the basement membrane into the dermal layer.
As local invasion of a cancer is the single most predictive feature for metastases, Clark recognized that these melanomas were likely metastatic. At the time, the process of invasion was thought to be a key feature of metastatic cells. This should have been obvious. Dr. Clark, however, had another idea.
Cancer Cell Proliferation in the Mesenchymal Compartment
Back in the lab, Clark was exploring fundamental differences between the growth properties of melanomas derived from early, non-invasive lesions (so-called Radial Growth Phase; RGP) and advanced, invasive lesions (so-called Vertical Growth Phase; VGP). In vitro, these cell types showed little difference; in vivo it was only the cells derived from VGP lesions that could form tumors in mice.
This observation led him to consider that the ability of cancer cells to proliferate in the mesenchymal compartment of the skin, not necessarily the ability to get there, might be a key feature of metastatic cells.
This was supported by the fact that, when cancer cells metastasize, they do so to the mesenchyme of the secondary organ. For melanoma, being able to proliferate in the dermis was an absolute requirement to metastasis, because the cells would be faced with a very similar environment at the secondary metastatic site.
Invasive Cancers are Like Metastases Yet to Metastasize
As a brand-new PhD student studying cancer metastasis, one realization was a “light bulb” moment for me. I recall exactly when that light went on, during Dr. Clark’s lecture at the Gordon Research Conference on Cancer, in August, 1991. I realized that an invasive cancer was akin to a metastasis that hadn’t yet metastasized. A melanoma that was fully capable of proliferation in the foreign tissue compartment of the dermis, the mesenchyme of the skin, was therefore likely capable of proliferation in the mesenchyme of tissues anywhere else in the body.
Based on this realization, a number of things quickly became evident:
- This concept gave supported clinical observations that locally invasive cancers generally always had a poor prognosis, but not due to invasion. The cells had to be able to proliferate when they arrived at the metastatic site. (RGP melanoma cells, when transplanted into the subcutaneous space of a mouse, couldn’t grow tumors, while their VGP colleagues could.)
- It also implied that many more cells at the primary site were likely competent for metastasis than previously thought. Why is it then that metastasis is so inefficient? Refer to my previous discussion on Single Cell Analysis – metastases are clonal outgrowths and therefore must be derived from clonogenic cells.
- Finally, this concept re-prioritized the role of cellular invasion, motility, and proteolytic enzyme production (the subject of my doctoral thesis) in the process of metastasis. Unrestrained cell growth was still the deranged master behind cancer, and remained its Achilles’ heel.
I won’t speak for all cancer biologists, but for me these “light bulb” moments are singular events. Exactly as the analogy intended, these moments illuminate a fragment of understanding that was, just seconds prior, in the dark. In a flash, fresh connections are made, new conclusions are drawn, and in that same flash, common knowledge becomes the way I used to think.
Further Reading:
Herlyn et al. Biology of tumor progression in human melanocytes. Lab Invest 1987;56(5):461-74.