Post FDA Approval: CAR-T Therapy Key Facts
 A few weeks ago, the FDA issued a historic approval of the first cancer cell therapy using a chimeric antigen receptor (CAR) T cell, authorizing the use of tisagenlecleucel (Kymriah) for the treatment of patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
A few weeks ago, the FDA issued a historic approval of the first cancer cell therapy using a chimeric antigen receptor (CAR) T cell, authorizing the use of tisagenlecleucel (Kymriah) for the treatment of patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
This has been followed up with a second CAR-T approval of Yescarta, for certain types of non-Hodgkin lymphoma (NHL).
Using A Patient’s Own Immune Cells to Treat Cancer
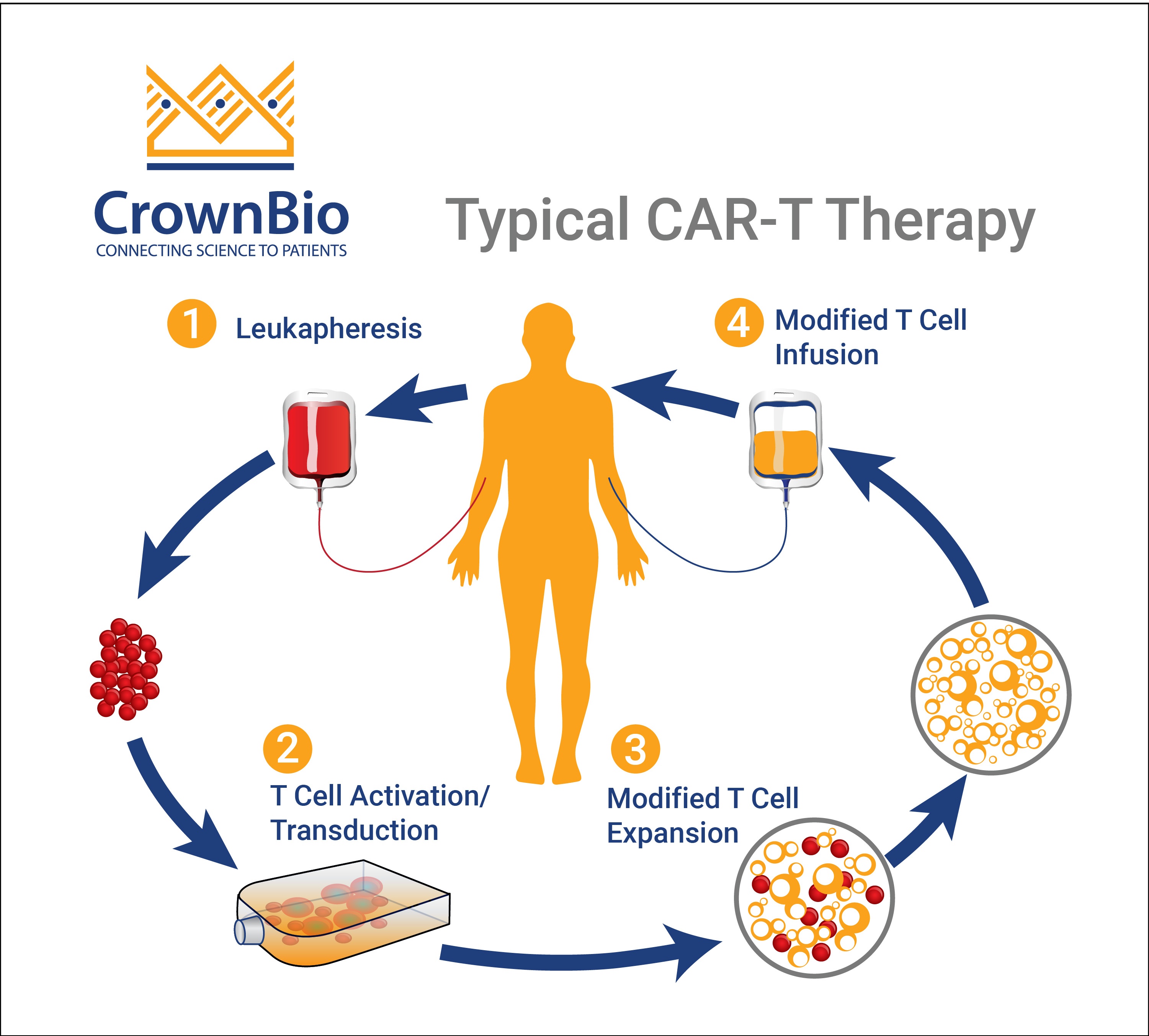
Cancer cell therapy is an exciting field, with promising results since it was introduced into clinical trials. Most of the cell therapies use a technique called adoptive cell transfer (ACT), collecting and using patients’ own immune cells to treat their cancer.
Different types of ACT can be distinguished using tumor-infiltrating lymphocytes (TILs), T-cell receptor (TCRs), and the chimeric antigen receptor (CARs), the first to enter clinical practice.
CAR-T Therapy – Optimized Over Multiple Preclinical Generations
A CAR-T therapy consists of engineered T cells that express a CAR on their cell membrane. The CAR protein fuses an extracellular antibody-derived specific tumor antigen recognition domain with internal TCR-derived activation domains.
The first generation of CAR-Ts contained only one activating domain and thus mimicked only TCR activation. Second (with one additional activating domain) and third generation (with two or more additional domains) CAR-Ts have additional costimulatory domains that further enhance the CAR-T cells’ ability to proliferate, expand and persist in vivo1. Most commonly, the costimulatory domains included are CD28 or 4-1BB (CD137).
The most common procedure for CAR-T therapy consists of the extraction of T cells from the own patient, which are then genetically modified and expanded in vitro. Finally, they are reinfused into the patient 2-14 days after lymphocyte depletion with conditioning chemotherapy, ready to fight the tumor. Persistence of CAR T-cells for as long as 3 years has been reported2.
CD19 is the Most Targeted Antigen for CAR-T Therapies
While CAR-T cells can (in theory) be redirected against any surface-expressed target of choice, most clinical trials so far have been directed to hematological malignancies. Today, 17 different CAR antigens are under investigation in 133 clinical trials for tumors of the hematopoietic and lymphoid system. The most frequently targeted antigen is CD19 with 56 ongoing and eight non-active trials3.
CAR-T Therapy of Solid Tumors has Proved Challenging
In the field of immuno-oncology, targeting solid tumors is a big challenge. Low T-cell infiltration and an immunosuppressive environment prevent the immune system from effectively attacking solid tumors. Moreover, CAR T-cell therapy to treat solid tumors has proved challenging because of the difficulty to identify target antigens on the surface of solid tumors that are not also expressed on normal tissues.
Nevertheless, 22 different CAR antigens are under investigation in 78 clinical trials. Previous trials focused on CEA as antigen-targeting colorectal, breast, and gastric cancer, adenocarcinoma as well as liver metastases. Ongoing trials target mesothelin, ErbB2/Her2, GD2 (neuroblastoma or sarcoma), or GPC3 (hepatocellular carcinoma) [3].
Most approaches to CAR-T engineer the patient’s own cells, but this process requires several weeks and is expensive. A possible solution is allogeneic CAR-T therapy, sourced from a healthy donor and ready to go when the patient needs it4.
Toxicity and Adverse Events Need to be Closely Monitored
CAR-T cell therapy can trigger a range of side effects, a particularly severe complication is cytokine release syndrome (CRS), also known as a cytokine storm. CRS is the result of T cell activation, so its presence actually indicates a positive response to therapy. CRS causes flu-like symptoms and can be fatal.
Neurotoxicity, which occurred after CAR-T cell infusion is also a common complication, named CAR-T-cell-related encephalopathy syndrome (CRES), which can sometimes lead to lethal swelling in the brain. Both CRS and CRES are treatable, with early identification important to swift improvement5.
Upcoming Approach Could Involve Modifying NK Cells
As mentioned previously, most of the cell therapy approaches are being carried out using modified T cells, but there is an increasingly interested in similar adaptation of the immune system’s “natural killer”, or NK cells, which are able to attack cancer cells directly and quickly, without the “priming period” required by T cells.
CAR-T Therapy: New Hope in Hard-to-Treat Hematological Malignancies
In summary, current CAR T-cell therapies represent a major advance in the treatment of hematological malignancies and with extensive efforts directed to currently incurable tumor types. The technology is not perfect, associated with severe and even life-threatening side effects, but it offers hope for patients that had none before. Definitely cellular therapy is an exciting field, where new and effective treatments will emerge in the upcoming years.
References and Further Reading:
- Gacerez et al. How Chimeric Antigen Receptor Design Affects Adoptive T Cell Therapy. J Cell Physiol. 2016;231(12):2590-8.
- Maude et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371(16):1507-17.
- Hartmann et al. Clinical development of CAR T cells—challenges and opportunities in translating innovative treatment concepts. EMBO Mol Med. 2017;9(9):1183-1197.
- Brudno et al. Allogeneic T Cells That Express an Anti-CD19 Chimeric Antigen Receptor Induce Remissions of B-Cell Malignancies That Progress After Allogeneic Hematopoietic Stem-Cell Transplantation Without Causing Graft-Versus-Host Disease. J Clin Oncol. 2016;34(10):1112-21.
- Kroschinsky et al. New drugs, new toxicities: severe side effects of modern targeted and immunotherapy of cancer and their management. Crit Care. 2017 14;21(1):89.
Cite this Article
Bourré, L., (2017) Post FDA Approval: CAR-T Therapy Key Facts - Crown Bioscience. https://blog.crownbio.com/car-t-cell-therapy-overview