 Explore how different imaging modalities are used to monitor in vivo immuno-oncology (I/O) studies in syngeneic tumor models.
Explore how different imaging modalities are used to monitor in vivo immuno-oncology (I/O) studies in syngeneic tumor models.
Why Use Imaging in Immuno-Oncology Studies?
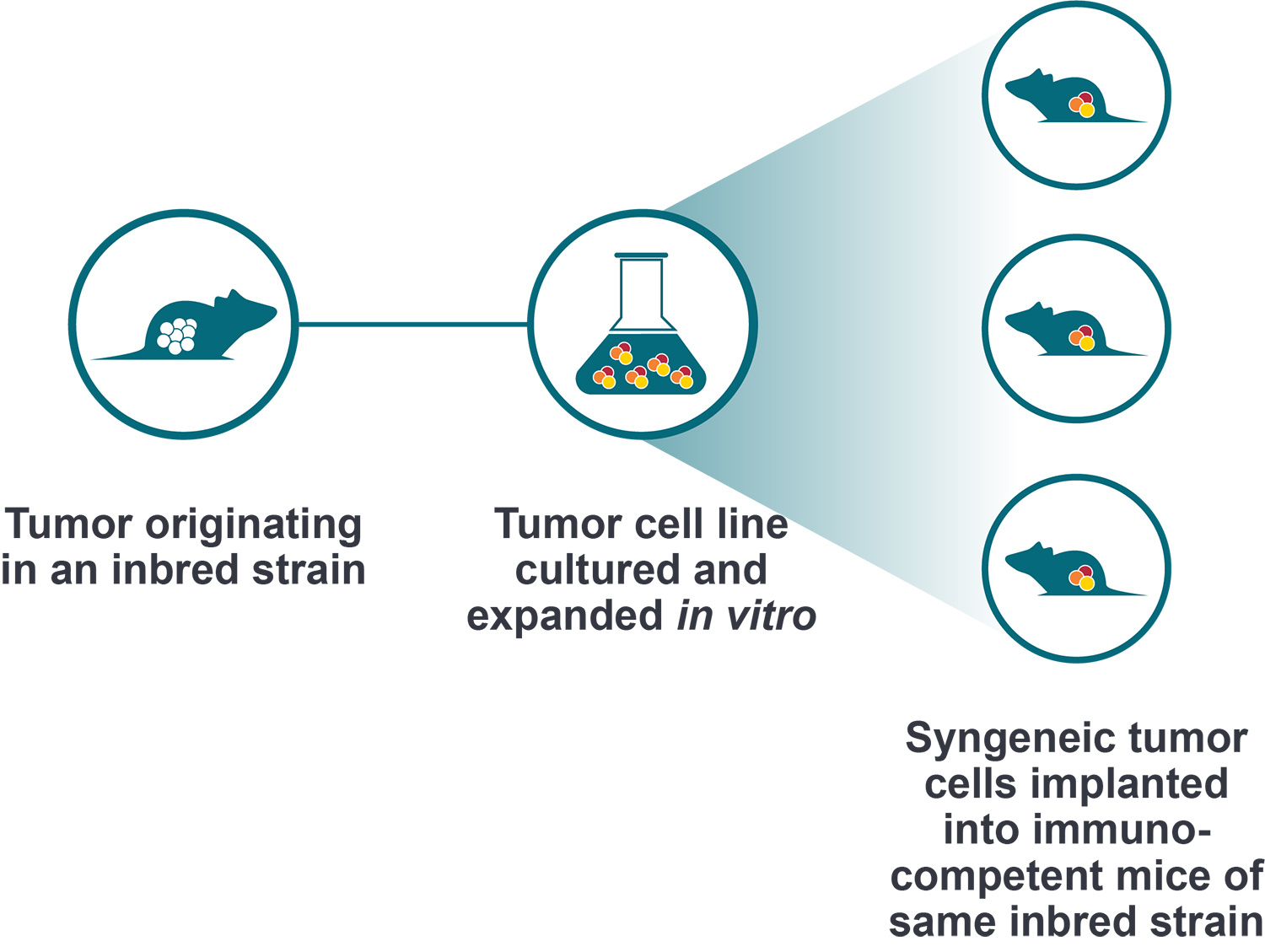
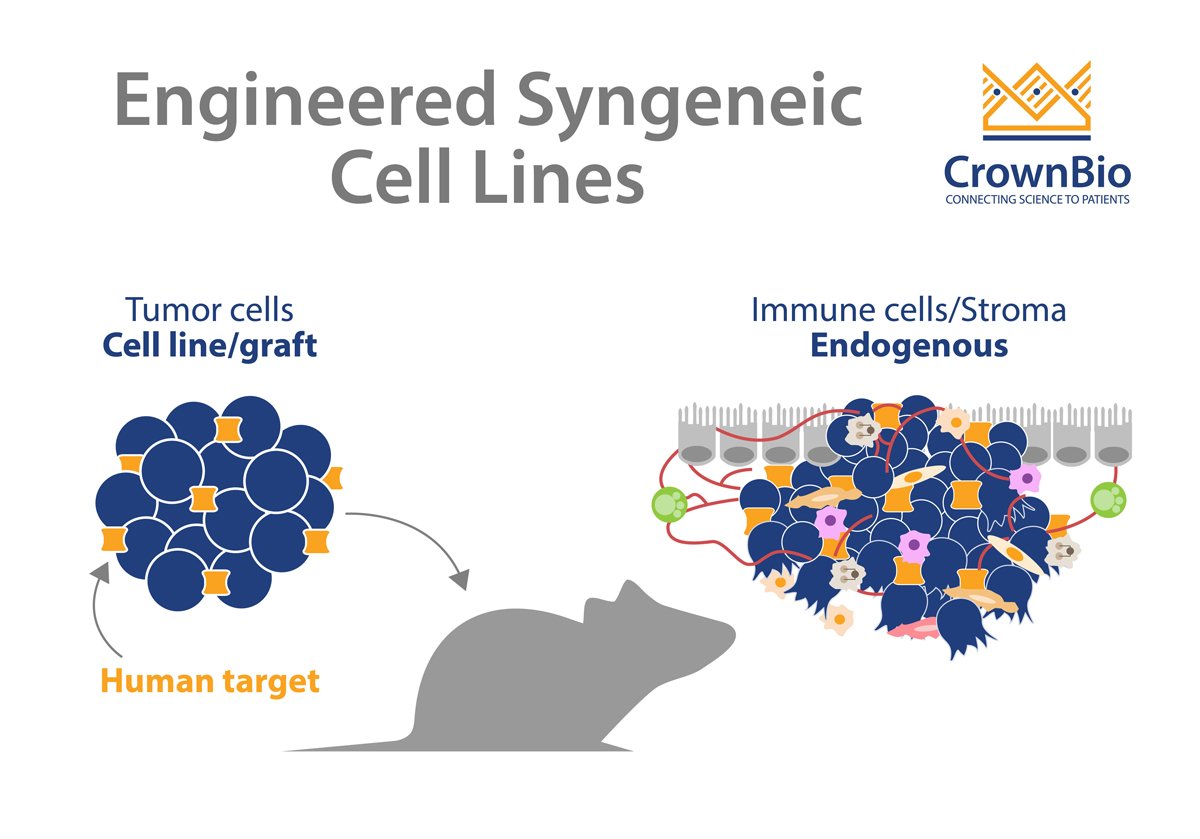
Immunotherapies are designed to improve the ability of the immune system to recognize and eliminate tumors. Syngeneic tumor models are widely used in preclinical I/O studies because they have an intact and functional immune system. This important feature allows researchers to study novel immunotherapies in the context of an in vivo immunocompetent model which recapitulates the interactions existing between the immune system and tumors. Furthermore, syngeneics are known to respond to clinically relevant immunotherapies, both in combination and as monotherapies.
Orthotopic models are commonly used in syngeneic tumor systems since they provide an environment with a higher burden for therapeutic penetrance into the tumor. In addition, the tumor microenvironment (TME) is thought to be more contextual in an orthotopic setting (as compared to the subcutaneous setting). This is valuable in preclinical studies since there are I/O therapies that elicit their efficacy by increasing the presence of immune cells in the TME.
Therefore, being able to non-invasively monitor tumor burden and the trafficking of immune cells to the tumor site(s) in I/O studies not only facilitates mechanism of action and pharmacodynamic studies, but can also reduce animal use and study costs.
While technological advancements have led to many possible imaging modalities to choose from, there are three that are commonly used in I/O tumor models that allow tracking of both tumor and immune cells:
- Positron Emission Tomography (PET)
- Bioluminescent Imaging (BLI)
- Fluorescent Imaging
The following provides a high-level overview of these three technologies, including some of their advantages and disadvantages that should be considered before choosing the right approach for your study.
Positron Emission Tomography (PET) Imaging
The use of PET imaging in preclinical immunotherapy studies typically involves the labeling of an antibody/protein with a PET radionuclide (e.g. Zr-89, F-18, Ga-68, Cu-64). Once the antibody binds its target, the decaying radionuclide is detected via a so-called coincidence event, which provides the precise location of the bound antibody molecules.
Advantages of PET Imaging:
- Therapeutic antibody can be used as an imaging probe
- Tumor burden can be monitored using a tumor-specific imaging probe
- Metastatic lesions can be localized
- Highly sensitive (since it relies on radionuclide decay)
- Immune cells can be tracked by using specific immune-cell probes
- Depth of imaging is not a concern due to minimal attenuation of signal
- Tomographic images can be produced
- Ex vivo imaging is possible
- Non-engineered cell lines can be used
- Reporter genes that double as suicide genes for adoptive therapy can be used
- Off target binding and excretion of therapeutics can be assessed
Disadvantages of PET Imaging:
- Investment in capital equipment
- Radioactive license and appropriate shielding of laboratory space and personnel is required
- Multiplexing is not simple since it cannot differentiate between two different nuclides in the same experiment
- Reporter gene may be immunogenic
Bioluminescent Imaging (BLI)
In vivo BLI is a popular imaging choice largely because it is relatively easy to use and has high sensitivity. This technology relies on the expression of a reporter gene that codes for a light-generating enzyme such as firefly, Renilla, or Gaussia luciferase in the tumor/immune cell of choice.
In the presence of the appropriate exogenous substrate, such as D-Luciferin or Coelenterazine, the luciferase converts chemical energy into visible light which is detected using cameras and allows the location of the engineered cells to be determined. Notably, some luciferases (such as Gaussia) can be secreted into the bloodstream which allows for estimation of tumor burden based on the blood levels of luciferase.
Advantages of BLI:
- Relatively inexpensive
- Non-radioactive
- Highly sensitive
- Useful to monitor tumor burden and location
- Useful to track immune cells
- Ex vivo imaging is possible
- Multiplexing is possible by using different luciferases that require different substrates
Disadvantages of BLI:
- Requires engineered cells
- Cannot track therapeutics and therefore cannot determine if it reaches the intended site of action
- Luciferase may increase immunogenicity of engineered cells
Fluorescent Imaging (FI)
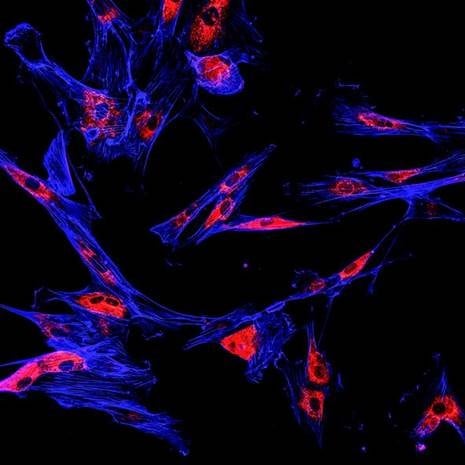
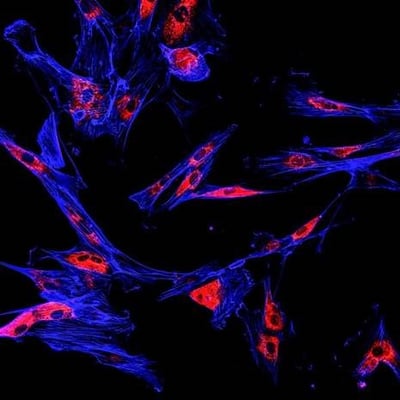
In vivo FI is widely used because of its high specificity and the availability of several different chemical and genetic (e.g. GFP, RFP) fluorophores that can be used to label a target (i.e. cells or antibodies) of interest. When the fluorophores are excited by specific wavelengths of light, they in turn emit light within a range of wavelengths that is collected using a detector that registers emission photons. There are also fluorophores that emit in the near-infrared portion of the spectrum which reduces the attenuation seen with white light (BLI) imaging.
Advantages of Fluorescent Imaging:
- Relatively inexpensive
- Both cells and antibodies can be labeled
- Conjugation to antibodies is straightforward
- Non-engineered cell lines can be used
- Metabolic processes and physiological conditions (e.g. intra-tumor pH) can be measured
- Models can be engineered with cell-specific fluorescent proteins (e.g. to track specific immune cells)
- Deep tissue imaging is possible using near-infrared probes
- Multiplexing is possible
- Tracking therapeutics is possible
Disadvantages of Fluorescent Imaging:
- Engineered cells may increase immunogenicity
- Least sensitive of the three imaging modalities
Conclusion
Molecular imaging modalities are highly useful for preclinical immuno-oncology studies because they allow for the tracking of both tumor and immune cells. The three most commonly used methods (PET, BLI, and FI) each have their own benefits and limitations which should be taken into consideration before selecting a platform for any given study. This will maximize the likelihood that the optimal imaging technology will be selected for the specific research questions at hand.