Regulatory T cells (Treg) are a specialized type of immune cells, crucial for the maintenance of immunological self-tolerance, the suppressive mechanisms thanks to which our body avoids self-destruction by an overactive immune system. Treg cells are also abundant in the tumor microenvironment where they can expand and differentiate into an immune-suppressive subpopulation. A study recently published on Science uncovered a new mechanism that allows Treg to keep a steady inhibition of the immune response, thereby protecting normal tissues. This mechanism could also be at play in the tumor microenvironment resulting in immune cells inhibition and tumor growth.
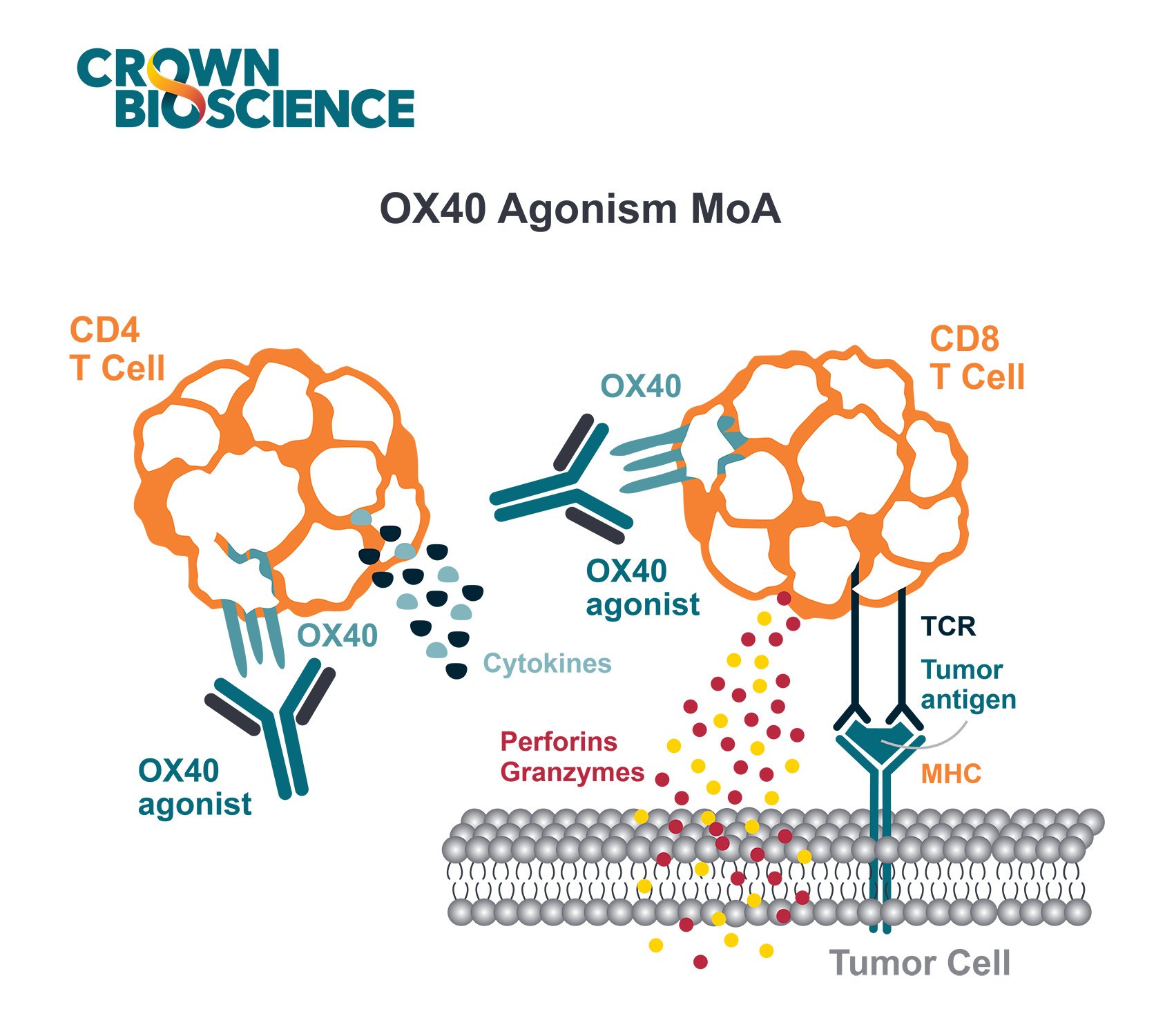
T cells are the immune system soldiers. They mature within the thymus, express on their surface a key molecule called T-cell receptor (TCR) and differentiate into various subsets. Effector T cells (Teff) undergo rapid changes in response to infection or pro-inflammatory signals to target specific pathogens or foreign bodies, while Treg' role is to prevent Teff from damaging normal tissues. The groups headed by Harvey Cantor, MD at the Dana Farber Institute and Harvard University recently reported that Treg express the Helios transcription factor, a protein that modulates gene expression. The study reports that Helios expression is paramount for Treg regulatory activity on Teff and to prevent autoimmunity in mice. When mice are incapable of expressing Helios, they develop an unstable Treg phenotype – when their immune system is challenged by infection – whereby activated Treg differentiate into Teff, mounting a strong immune response that can no longer distinguish between foreign bodies and self-tissue. This terminal differentiation of Treg into Teff and the consequent suppression of self-tolerance seems to involve the inhibition of an important pro-inflammatory factor known as STAT5.
While this is an unwanted response during infection, this mechanism could become advantageous when fighting cancer. This is the hypothesis that Cantor and his colleagues are now exploring while applying their mechanistic findings to the treatment of cancer. Cancer cells have the ability to evade the immune system by disguising themselves as normal cells or, as Cantor suspects, by producing molecules that attract Treg in great numbers to the tumor. A high Treg concentration in the tumor microenvironment could in turn attenuate the Teff' response allowing tumor cell survival.
Experiments in mice injected with metastatic melanoma cells show that animals unable to produce Helios developed far fewer cancerous nodules than normal mice, and survived far longer. Several studies also indicate that while tumor associated Treg express high levels of Helios, the expression of this transcription factor in peripheral Treg is generally very low. This is a crucial point since it implies that if we could target Helios, or genes in the Helios pathway, by antibodies or small-molecules we could prevent tumor associated Treg from inhibiting the immune system activation against cancer cells, while potentially leaving the population of circulating Treg unaffected, producing fewer immune-related side effects.
Last but not least studies on colorectal cancer show that the majority of tumor associated Treg also express high levels of the checkpoint inhibitor CTLA-4, further suggesting possible therapeutic interventions in combination with the popular anti-CTLA-4 antibody.
Crown Bioscience looks forward to future therapeutic developments exploiting this newly identified mechanism of immunomodulation. The lack of experimental immunotherapy models with a functioning immune system represents a major obstacle for the testing the efficacy of new immunotherapies. At Crown we support research in immuno-oncology utilizing a range of platforms, with either murine or human immunity. Our immunotherapy resources include syngenic (bioluminescent and metastatic) models, GEMM, MuPrime™ (the murine version of HuPrime®, the world’s largest collection of well-characterized and validated Patient-Derived Xenograft models), HuMice™ (humanized mice produced through inoculating human hematopoietic cells into immunocompromised mice), and MiXeno™ (creating transient human immunity by mixing human peripheral blood mononucleated cells with xenograft models). We also support preclinical drug development through the use of our in vivo grade human and mouse isotype control antibodies.
Contact us today at busdev@crownbio.com to discuss how our immunotherapy platforms can help advance your drug discovery program.