Cancer cells have the ability to evade the immune system by exploiting a self-regulatory mechanism that immune cells use to avoid attacking healthy cells. Luckily we now understand how to therapeutically reverse this immune escape, and researchers have developed innovative antibodies that target the inhibitors present on the tumor surface (e.g. anti-PD-1/PD-L1 or anti-CTLA-4). A new study in preclinical models has recently demonstrated that the conventional chemotherapeutic cyclophosphamide can be efficacious as an anticancer agent if used in combination with immunostimulatory Toll-like receptor agonists.
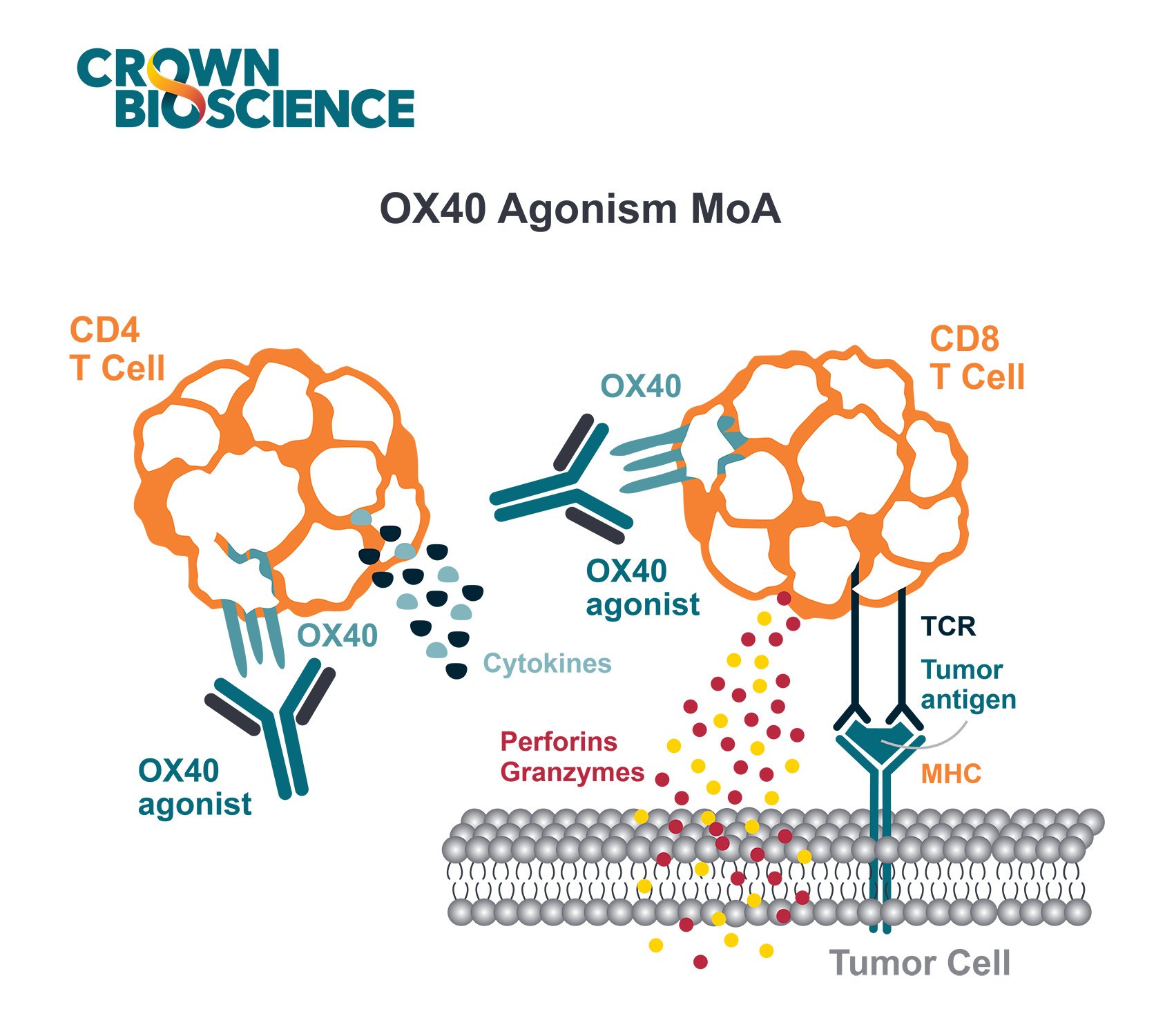
Immune cells are the army that keep our bodies clear from foreign pathogens or terminally damaged cells. Normal, healthy cells are spared by the immune system thanks to the presence of specific molecules such as PD-L1, B7-1, B7-2, etc on their surface that prevent the immune cells from becoming activated.
Bacteria, virus-infected cells, or cancer cells on the other hand are detected as foreign bodies and destroyed. Cancer cells, however, have evolved to evade this control by expressing on their surface the same inhibitory molecules as normal, healthy cells, stopping the immune cells from killing them. This cancer-dependent immunosuppression can be reversed with the use of therapeutic antibodies. The antibodies counteract the immunosuppressive activity of molecules like PD-L1, B7-1, or B7-2 on the tumor by preventing them from binding to their natural partners on the surface of the immune cells.
Additionally, specific populations of immune cells (i.e. myeloid-derived suppressor cells – MDSCs, or regulatory T-cells – Treg) are responsible for tuning down the effector killer cells (Teff) to avoid collateral damage in normal surrounding tissues, acting as sentinels against an uncontrolled activation of the immune system.
How does Chemotherapy Work in Treating Cancer?
Chemotherapy is a term used to refer to a large class of agents that non specifically kill dividing cells, such as tumor cells, based on their ability to induce DNA damage. Because of the lack of specificity during this process, most chemotherapeutic agents also damage other healthy cells in the body, like cells in the hair follicles or some immune cell precursors that, contrary to the majority of cells in an adult organisms, still retain the ability to replicate.
Cyclophosphamide, for example is a commonly used chemotherapeutic, which was shown to deplete patients of MDSCs and Treg, thus potentiating the antitumor response by the Teff.
In a new study published in Oncotarget a Mayo Clinic research group set out to find whether they could come up with a combination treatment strategy to further potentiate the antitumor effect of cyclophosphamide.
Using preclinical models of breast, prostate, and colorectal cancer (the syngeneic 4T-1, Panc02, and CT26 models), the group found that co-administering an agent able to emulate a life-threatening bacterial infection potentiates the efficacy of cyclophosphamide.
This bacteria-like agent awakens the immune system of tumor bearing animals by activating the Toll-like receptor (TLR) pathway which, when combined with cyclophosphamide immunoregulatory properties, results in a well-tolerated therapeutic synergy that permanently eradicates advanced tumors.
These results further demonstrate that fighting cancer by taking advantage of a patient’s own immune system could represent a valuable approach to cancer treatment.
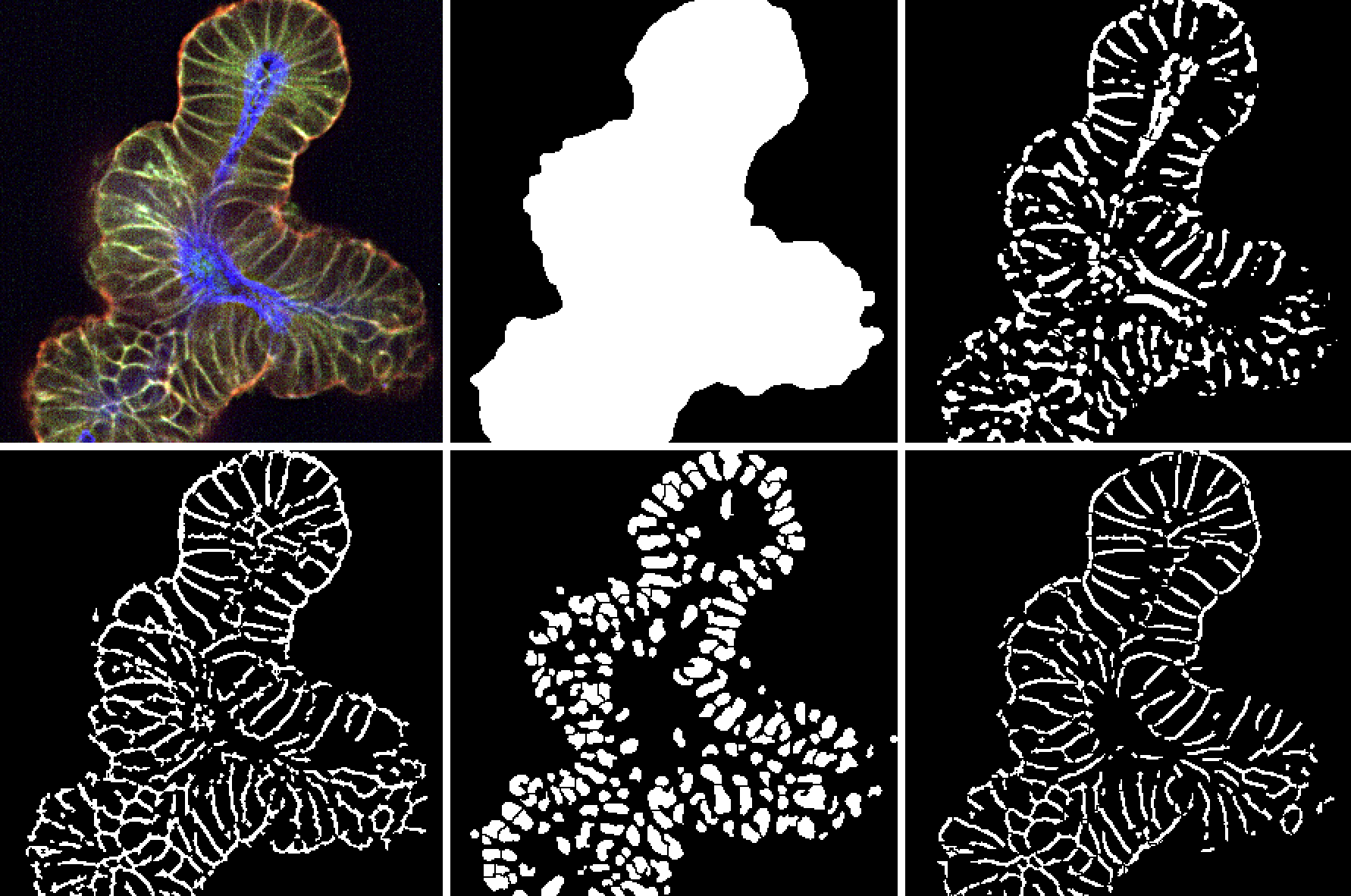
To help drive forward immunotherapy research, develop new treatment strategies, and recapitulate clinical treatments, experimental immunotherapy models are needed. The Mayo Clinic study used syngeneic models, which are allografts derived from immortalized mouse cancer cell lines in a recipient host with a fully competent immune system.
CrownBio has validated a range of syngeneic models that we have extensively profiled for in vivo response to a variety of immunotherapeutics, providing clients with the information necessary to select models and the correct doses for combination strategies. We have also generated detailed expression maps and mutational profiles of syngenic tumors before treatment that may be useful for combination studies of targeted agents and immunotherapy or to identify biomarkers that predict response to different immunotherapies.
To evaluate pharmacodynamic effects or efficacy of immunotherapeutic agents across multiple cancer types, CrownBio has recently launched MuScreen™, a large-scale, staggered, in vivo screening of syngeneic models that provides a cost effective approach to fast track strategies.
Contact us today to learn more about our collection of syngeneic model or to enroll your compounds into MuScreen.