 As immunotherapeutics continue to dominate oncology headlines and research, more preclinical studies are requiring immunocompetent models. Syngeneic models (recently reviewed in this post) of murine immunity have become somewhat of an I/O workhorse, but when human-specific therapeutics need to be assessed human targets (and therefore humanized models) are required.
As immunotherapeutics continue to dominate oncology headlines and research, more preclinical studies are requiring immunocompetent models. Syngeneic models (recently reviewed in this post) of murine immunity have become somewhat of an I/O workhorse, but when human-specific therapeutics need to be assessed human targets (and therefore humanized models) are required.
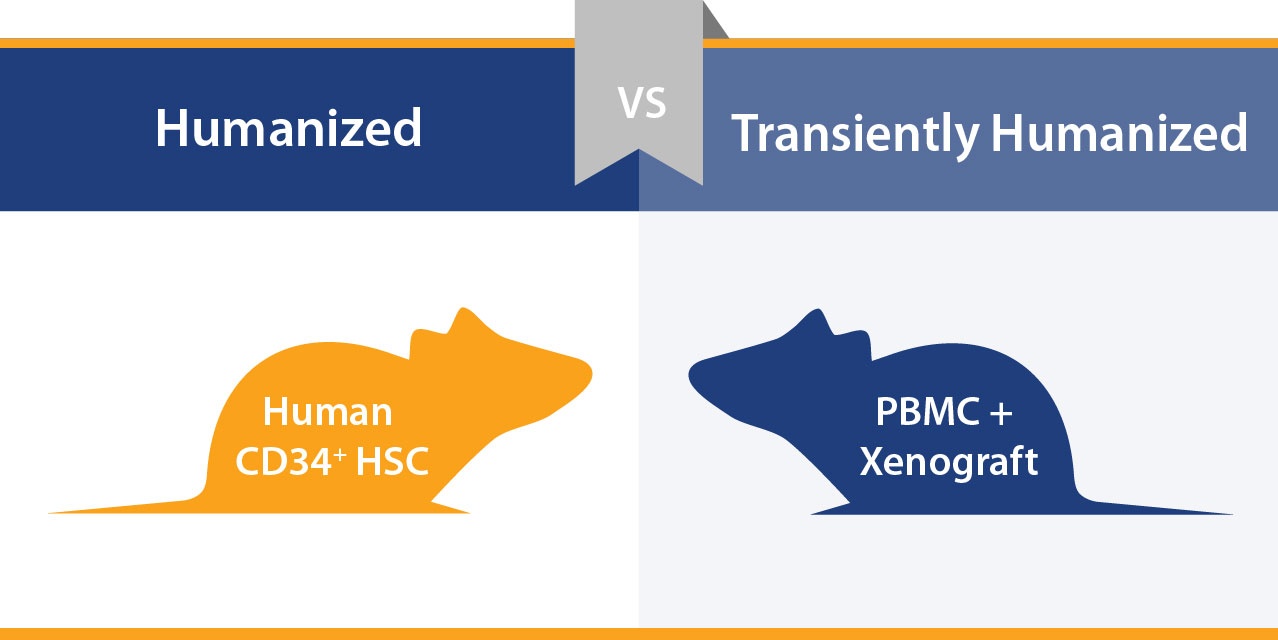
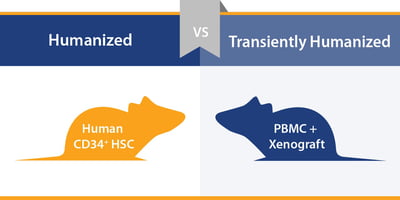
There are two main options when humanized models are needed – stable humanized mice or a more transient, partially reconstituted model. This post takes a look at each model type and when you might use them for a particular study.
Humanized Mouse Models Develop Multiple Aspects of Human Immunity
There are a number of humanized mouse models available for immunotherapy assessment, based around the engraftment of human CD34+ hematopoietic stem cells into highly immunodeficient mice such as the NOG mouse available from Taconic and the NSG™ from The Jackson Laboratory.
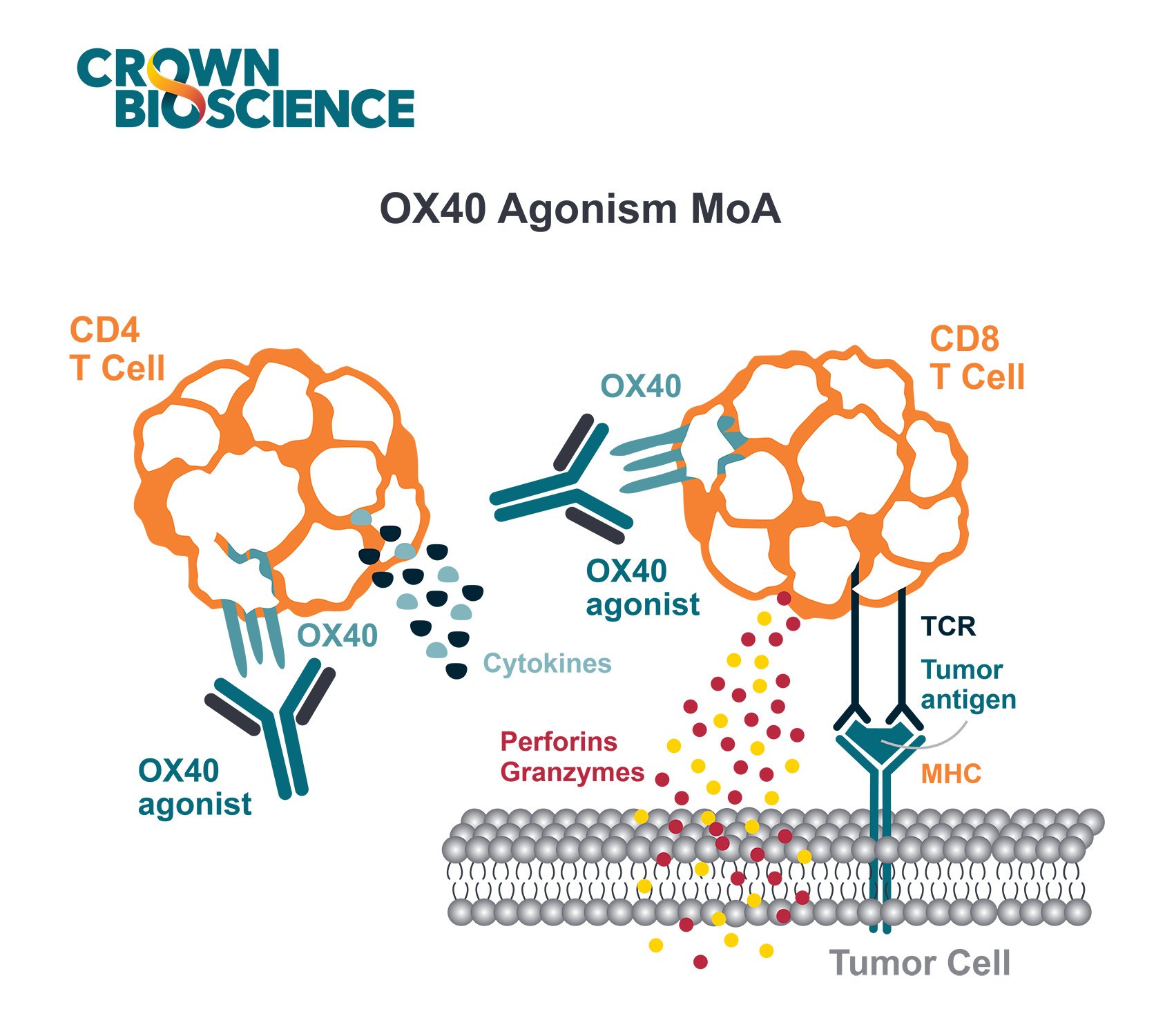
The resulting models display robust human T cell generation, recapitulating the human T cell profile quite well, including CD4+ helper cells, CD8+ cytotoxic T lymphocytes, and Treg cells. B cells are also present, along with lower levels of NK cells (although these cells may not function well) and macrophages.
Next generation models have also now been established to support further immune cell development, including improved NK cell and myeloid lineage expression.
Add Xenografts for a Human:Human System
These models can then be engrafted with human tumors to provide a system that is ideal for targeting T cells – with human targets, stroma, diversity of lymphocyte response, and a human immune response. This means that a range of human-specific therapeutics can be assessed.
One main use of this model type is with patient-derived xenografts (PDX) to provide data for clinical trials.
Humanized PDX – Highly Predictive Immunotherapy Efficacy Testing
PDX are generated from patient tumor tissue directly implanted in mice, and are never grown or manipulated in vitro. They more closely recapitulate parental tumor heterogeneity and characteristics than traditional xenografts, and are regarded as the most predictive preclinical oncology model.
Large PDX panels represent the diversity of tumors seen in the clinic, and can be used in population studies with humanized mice to evaluate large scale, human-specific immunotherapy response. Data on responders and non-responders can be used to generate patient stratification guidance for later clinical trial, hopefully improving chances of clinical success.
Limitations: Complex Models, Producing Costly Studies
As with all models, humanized mice do have drawbacks. Donor variability occurs which needs full characterization, the full immune system is not recapitulated, and some immune cells may not be fully functioning (e.g. B and NK cells as discussed above).
Compared with models such as syngeneics, humanized mice are complex to use, producing difficult to run studies, which involve a high cost for researchers. But, humanized models are still needed for human-specific therapy assessment.
This has led to the development of transiently humanized mice – a simplified system of humanization to reduce costs and complexity.
Transiently Humanized Models – A Straightforward Approach to Humanization
Transiently humanized models are created via a much simpler approach – peripheral blood mononucleated cells (PBMC) are combined with traditional, cell line derived xenografts, either admixed or sequentially, and added to immunodeficient mice.
Partially reconstituted immunity is achieved, and provides a system for investigating mature lymphocytes in a quick and robust model. In these models, B cells show antigen response under some circumstances, although B cells levels in peripheral blood are insignificant. It’s a perfect approach for:
- Studies on short timelines, needing a faster study than using full humanized models
- High throughput assessment of I/O agents
- Initial agent selection or stratification before moving onto a full humanized study
Models have been developed for a range of cancer types, including both solid tumors and blood cancers, providing a versatile option for when a simple humanized model is needed.
Beware Graft versus Host Disease
As with fully humanized models, transient models obviously have limitations. The main issue here is graft versus host disease (GvHD) which is driven by the presence of mature T cells. This can mean a very limited treatment window to carry out studies, sometimes as little as 10 days to 3 weeks to perform efficacy studies. Models are being developed to address the shortcomings of this model, such as the B2m -/- mouse.
While both model types have their pros and cons, together they provide a platform that can hopefully provide a humanized model type for any given human-specific I/O study.