 When are patient-derived xenografts most useful in your drug development pipeline?
When are patient-derived xenografts most useful in your drug development pipeline?
Anyone working in preclinical and translational oncology drug development will seen and use treatment data from xenograft studies. Historically, this data originated from ‘traditional’ cell line derived xenografts (CDX), which use cell lines immortalized in vitro from patient tissues.
Now, with patient-derived xenografts (or PDX) derived directly from implanting patient tumor tissue into a mouse, many researchers face the question of which is the ‘right’ xenograft to use, or when should PDX be added into their preclinical oncology development program.
Cell Line Derived Xenografts – Early Stage Proof of Concept Development Tools
Traditional xenografts are excellent tools for early stage drug development. When looking for proof of concept as to whether your new agent works in a specific indication, or against a specific overexpressed protein, xenografts can be rapidly run and compared with a wealth of historic data. Typical uses might include:
- Initial evaluation of multiple potential candidates or compound series
- To evaluate and rank efficacy of a new agent against a known cell line target
- To understand aspects of new drug properties or MOA
Moving to Clinical Trial? Move to PDX Models
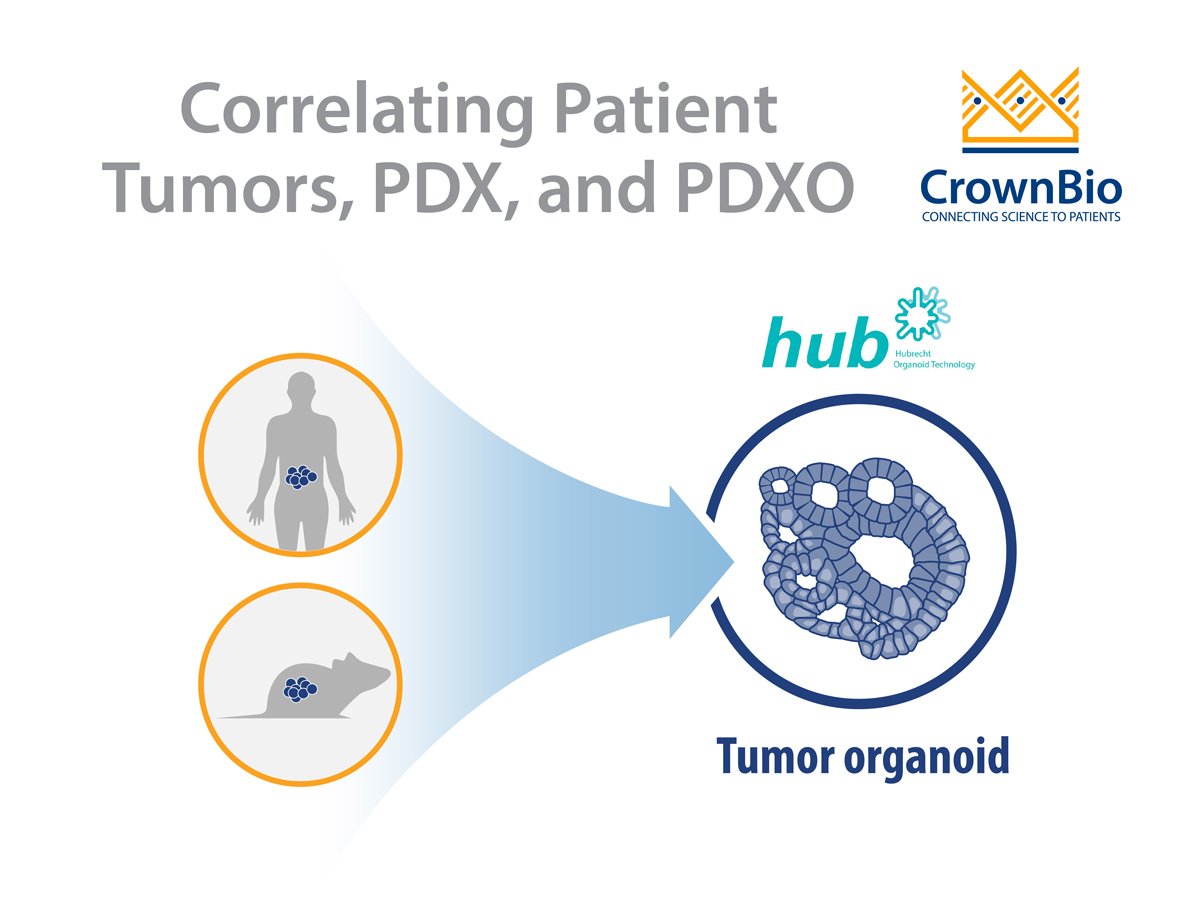
The main benefit of PDX models over traditional xenografts is their predictability of response. Closely recapitulating patient tumors for both histo- and molecular pathology, PDX growth and response to SoC have been shown to highly correlate with patient clinical response. PDX are therefore ideal tools to use when gearing up for clinical trials, where highly predictive response data is needed for guidance on indication or patient stratification.
There are two main ways to use PDX at this stage:
- At an individual model level to study specific tumor response
- A population study to predict clinical response rates
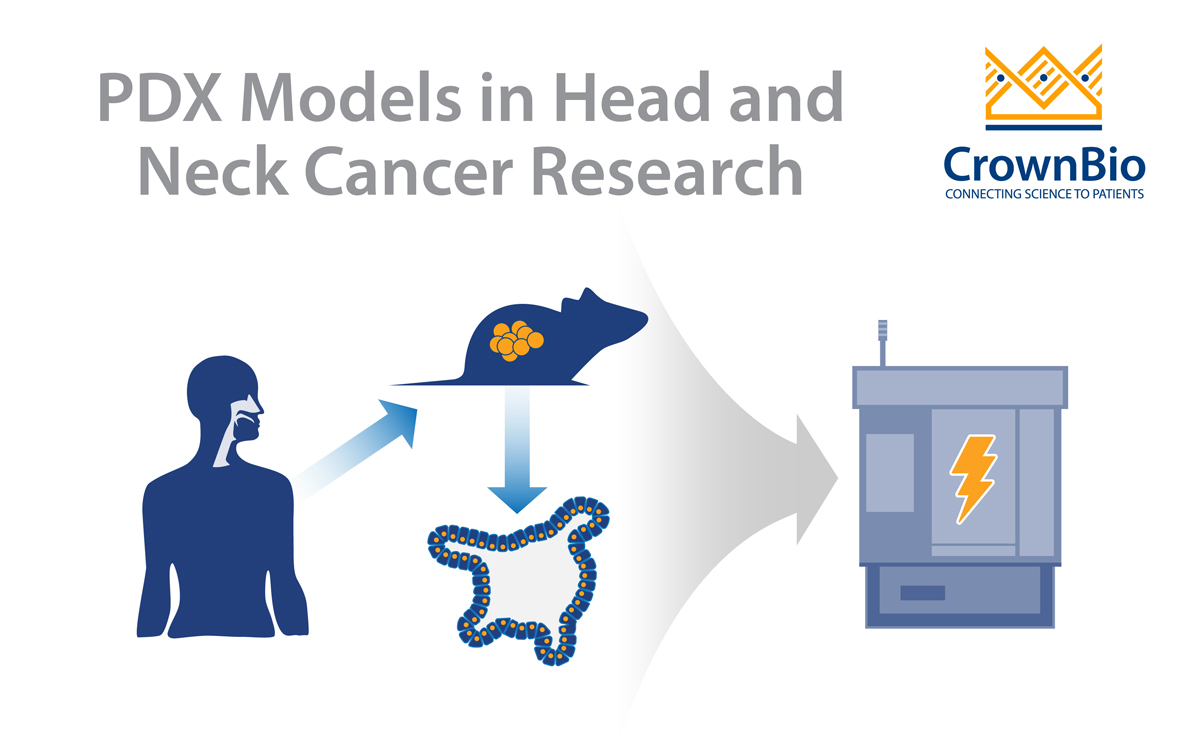
Using Individual Models to Study Tumor Response
To confirm tumor response, or to study specific combination therapies, small numbers of unique PDX models can be used. These PDX are specifically chosen based on a molecular target of interest, e.g. EGFR gatekeeper mutation, to evaluate response to an agent, and to verify drug sensitivity already seen at an in vitro or cell line derived xenograft level.
This can confirm specific agent efficacy against a clinically relevant mutation, overexpression, or fusion in a xenograft truly reflecting the clinical situation.
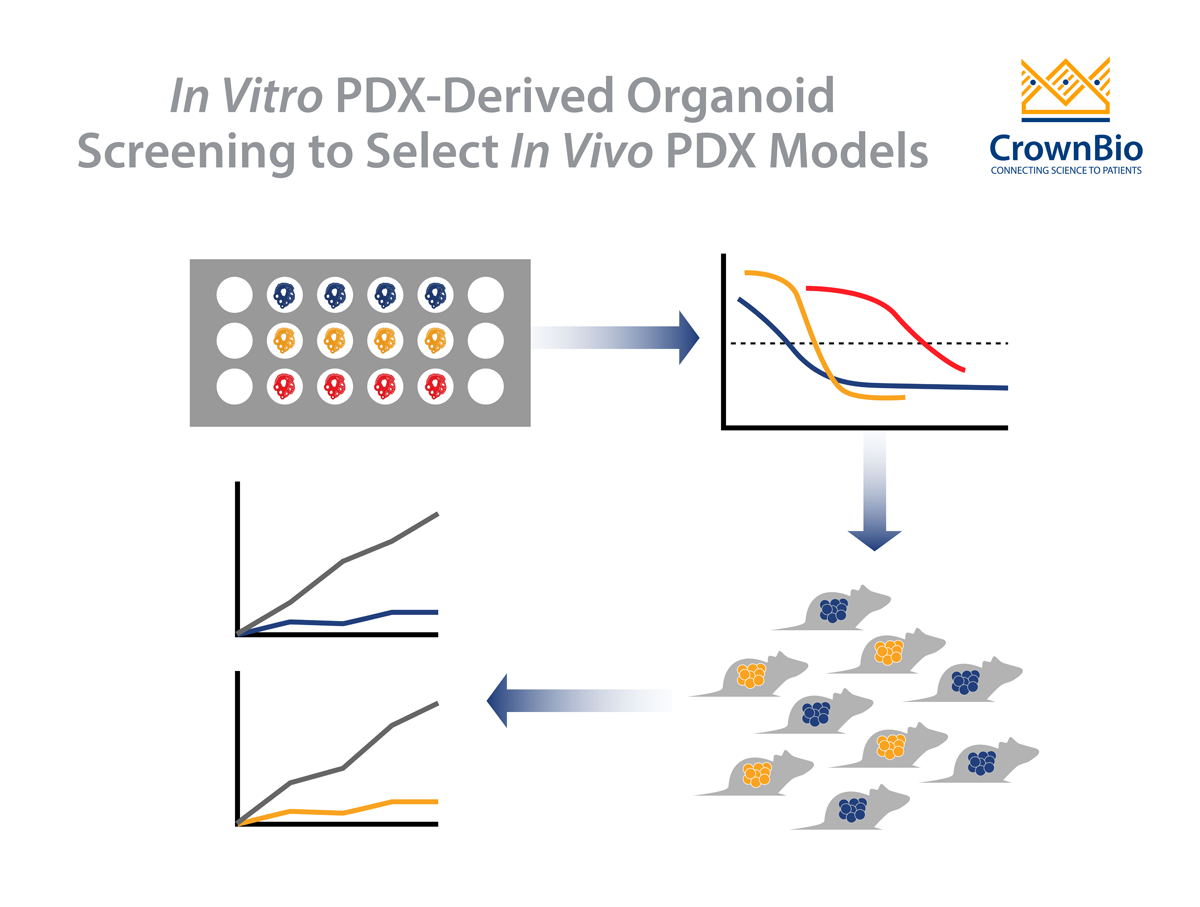
Population Studies to Predict Clinical Response
When planning for clinical trials, correct indication and patient stratification is essential to ensure maximum success. PDX can also be used to model population responses rather than individual models.
Large numbers of PDX can be used to represent the oncology patient population diversity, establishing response rates to an agent or combination treatment across the population. This can then be used to guide the correct indications for clinical study.
Well-characterized models can also be exploited to compare response against PDX genetic features across the population, providing predictive biomarkers and signatures which can stratify clinical patients to include only those with a good chance of success.
Complementary Xenograft Tools for a Comprehensive Drug Discovery Program
While these suggestions don’t constitute an exhaustive list of drug development applications for patient-derived and cell line derived xenografts studies, they hopefully provide a brief guide for those unsure on the best way to integrate PDX into their programs and show how the two xenograft types can be combined to inform more efficient drug development programs.