Checkpoint inhibitors are the most heralded drugs in oncology. They work by removing the brake on the immune system to promote its activation. In other words they block the molecules that switch off immune cells. However the early results of a recent Phase I study sponsored by Pfizer revamped some interest around therapies that take the opposite approach: keep the activating receptor on the immune cells constantly switched on.
The use of an anti-4-1BB antibody as an anticancer agent locking the immune cells into an active state was showed by Dr. Lieping Chen back in 2002. 4-1BB is the natural ligand for the CD137 receptor and it is mostly expressed on the surface of antigen presenting cells, like dendritic cells (DCs). DCs engagement is essential to obtain a full immune response. Once they recognise the presence of a foreign body, such as a pathogen or a cancerous cells the level of 4-1BB expressions dramatically increases on their surface. The crosslinking of 4-1BB with CD137 on the surface of T cells leads to T cells multiplication and activation and enables the immune system to kill pathogens or cancer cells.
On the basis of Dr. Chen’s work Bristol-Myers started a clinical trial for the use of an anti-4-1BB antibody (urelumab) that was terminated in 2008 after early data showed dangerous signs of liver damage. However scientists and clinicians have soon understood that a better dosing at the appropriate time could achieve the desired anticancer effect without the toxicity. Researchers at Stanford University Cancer Institute are now experimenting the combination of existing cancer therapies, such as Roche's Rituxan® (rituximab) to prime the immune system, with an anti-4-1BB antibody at very low doses to keep the immune system active.
Pfizer has recently reported early data of a new antibody treatment that targets 4-1BB with some phenomenal outcomes in patients whose lymphoma had stopped responding to any other available therapy. Nearly 40% of patients with follicular lymphoma and a third of those with mantle cell lymphoma saw a reduction in their cancer with no serious side effects. Pfizer has at least five more Phase I studies underway or in planning for solid tumors and blood cancers. According to Reuters, Bristol-Myers Squibb, Johnson & Johnson and AbbVie are doing early stage testing of their antibodies before starting human trials.
The early success of Pfizer’s anti-4-1BB therapy prompted Stanford researchers to test other combination therapy approaches. For example, they plan to test Pfizer's antibody with Roche's Herceptin (trastuzumab) in breast cancer, and Bristol's urelumab with Eli Lilly’s Erbitux (cetuximab) in colon and head and neck cancers.
The Pfizer results are promising and Crown Bioscience looks forward to seeing further data from advanced anti-4-1BB clinical studies. Although Phase I cancer trials have become better predictors of future results, because of our improved understanding of immunology and human genetics, a yet incredibly high percentage of the drugs that looked promising early, eventually fail when larger trials turn up safety problems or disappointing efficacy.
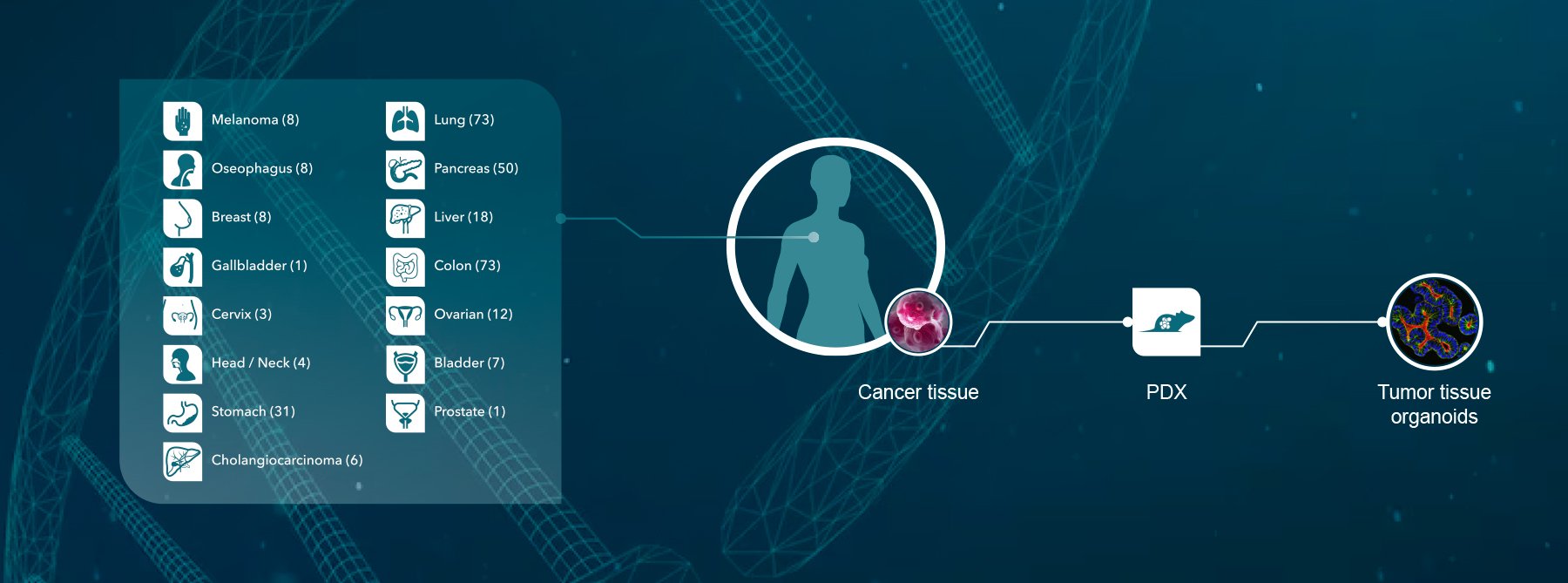
A lack of experimental immunotherapy models with a functioning immune system represents a major obstacle for the identifications of predictive biomarkers of response. Crown Bioscience supports research in immunotherapy with a range of platforms, with either murine or human immunity. Our immunotherapy resources include syngenic (bioluminescent and metastatic) models, GEMM, MuPrime™ (the murine version of HuPrime® which is the world’s largest collection of well-characterized and validated Patient-Derived Xenograft models), HuMice™ (humanized mice produced through inoculating human hematopoietic cells into immunocompromised mice), and MiXeno™ (creating transient human immunity by mixing human peripheral blood mononucleated cells with xenograft models). We also support preclinical drug development through the use of our in vivo grade human and mouse isotype control antibodies.
Contact us today at busdev@crownbio.com to discover how we can transform your immunotherapy research today.