Metastasis remains the main cause of cancer-related mortality, despite major scientific advances in the understanding of the molecular and genetic basis of cancer. The term metastasis refers to the spreading of cancer cells to peripheral tissues, which they colonize after shedding from primary tumors and travelling through the blood stream or lymphatic system. Understanding the mechanisms of metastasis initiation and progression is critical to developing new strategies to treat and prevent metastatic disease.
It is currently believed that cancer cells undergo a de-differentiation process called epithelial-to-mesenchymal transition (EMT) that reverts them into “cancer stem cells” and that EMT cells becomes “seeds” able to initiate and propagate metastatic tumors. However, the identification of these metastasis-initiating cells in human cancer remains a challenge, and only a partial EMT has been occasionally observed in vivo.
Most studies exploring the functional role of EMT in tumors have been developed in cell culture where EMT is artificially induced by loss-of-function and gain-of-function of key EMT inducing factors, whereas in vivo models in which to address a causal connection between EMT, invasion and metastasis are lacking.
Recent findings from two groups investigating the metastatic process in preclinical models of breast and prostate cancer are challenging the dogmatic view that EMT is required for epithelial tumors to metastasize.
The group headed by Dr. Dingcheng Gao at Cornell University, collaborating with teams from Columbia University, Houston Methodist Research Institute, and Soonchunhyang University in South Korea, devised a new approach called “EMT cell lineage tracing" to mark and follow the development of single breast cancer cells in mouse models of metastatic breast cancer. In these engineered models breast cancer cells are labeled with a red fluorescent marker, which turns green if they undergo EMT. Not surprisingly the group found that primary breast tumors contain a small proportion of cells that undergo EMT, however lung metastases mainly consist of non-EMT tumor cells that maintain their original epithelial phenotype.
They also found that lung metastases still develop when EMT is blocked in their models, suggesting that EMT is not required for tumor cells dissemination or peripheral tissues colonization. However EMT becomes key once animals are treated. While primary tumors respond to chemotherapy, cells that have undergone EMT are resistant to treatment and contribute to recurrent lung metastasis formation after chemotherapy. Treating breast cancer bearing animals with an EMT blocker together with standard chemotherapy abrogated this resistance and prevented the formation of metastasis.
These important findings were supported by a back-to-back publication on the same issue of Nature of similar data in a metastatic prostate cancer model, where EMT suppression leads to increase sensitivity to chemotherapy and increased overall survival.
These studies suggest a re-evaluation of the role of EMT in cancer progression. Epithelial cells could enter the bloodstream without transitioning to a mesenchymal state, by alternative means such as collective epithelial-cell migration or tumor fragmentation.
Most importantly they found that the EMT switch could prompt chemo-resistance. By transitioning to a mesenchymal state cancer cells become quiescent and refractory to drugs targeting actively dividing cells. A better understanding of how tumor cells transition to a mesenchymal state and how this process influences drug response is likely to provide fertile ground for drug discovery.
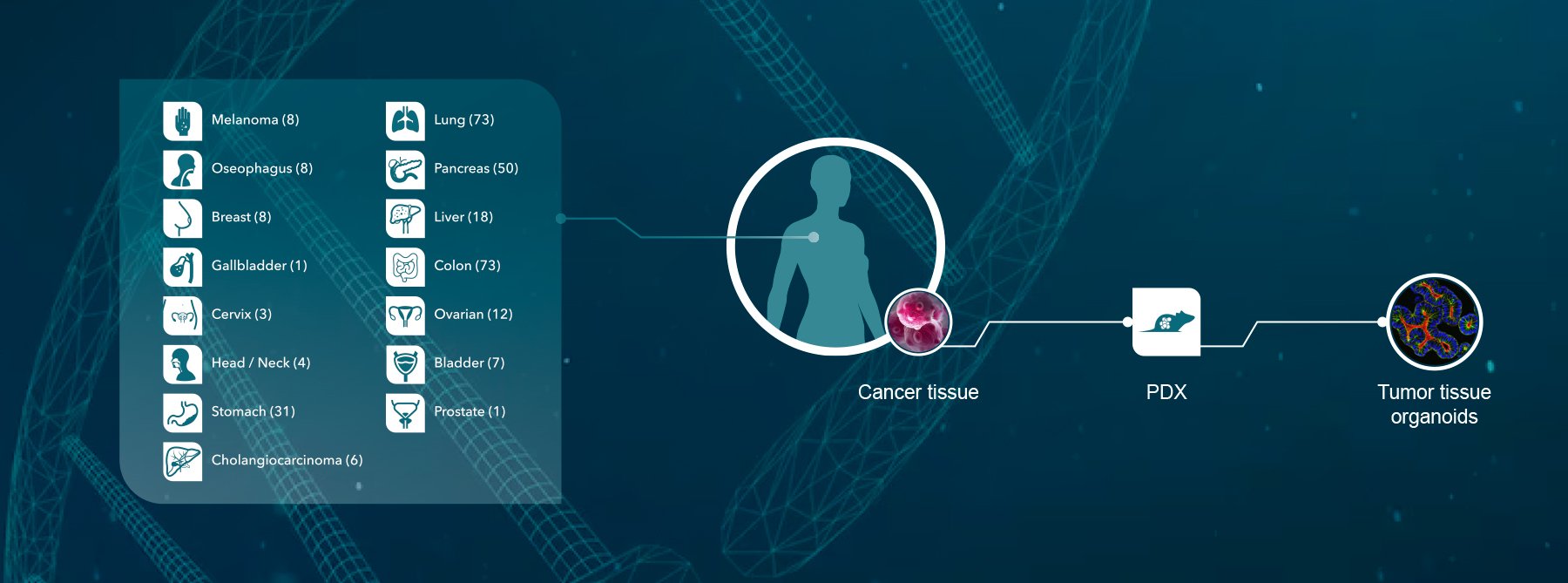
Crown Bioscience has a longstanding track record in prostate and breast cancer research with a range of research platforms available for all stages of drug development. Besides our OmniPanel™ and ValidatedXeno™ collections of breast and prostate cancer cell lines, we have developed several cell line derived xenograft (CDX) models, including orthotopic and bioluminescent models for imaging and metastatic disease evaluation.
Crown has also validated a comprehensive collection of PDX breast cancer models (HuPrime®) as well as models for Immunotherapy Research using mouse immunity (syngenic and MuPrime™). Models with human immunity (HuMice™) are currently under development.
Contact us today at busdev@crownbio.com for your copy of our Breast Cancer and Prostate cancer Application Notes or for a copy of our factsheet on the mBR6004 MuPrime model of metastatic breast cancer for Immunotherapy research.