 NSCLC patients with EGFR exon 20 insertions lack treatment options, partly due to a lack of patient genotype-relevant preclinical models for assessing novel agents. A new publication details the preclinical evaluation of osimertinib for this EGFR mutation type, using a series of CRISPR-Cas9 engineered cell lines and patient-derived xenograft (PDX) models harboring clinically relevant EGFR exon 20 insertions.
NSCLC patients with EGFR exon 20 insertions lack treatment options, partly due to a lack of patient genotype-relevant preclinical models for assessing novel agents. A new publication details the preclinical evaluation of osimertinib for this EGFR mutation type, using a series of CRISPR-Cas9 engineered cell lines and patient-derived xenograft (PDX) models harboring clinically relevant EGFR exon 20 insertions.
NSCLC Patients with Tumors Bearing EGFR Exon 20 Insertions Lack Treatment Options
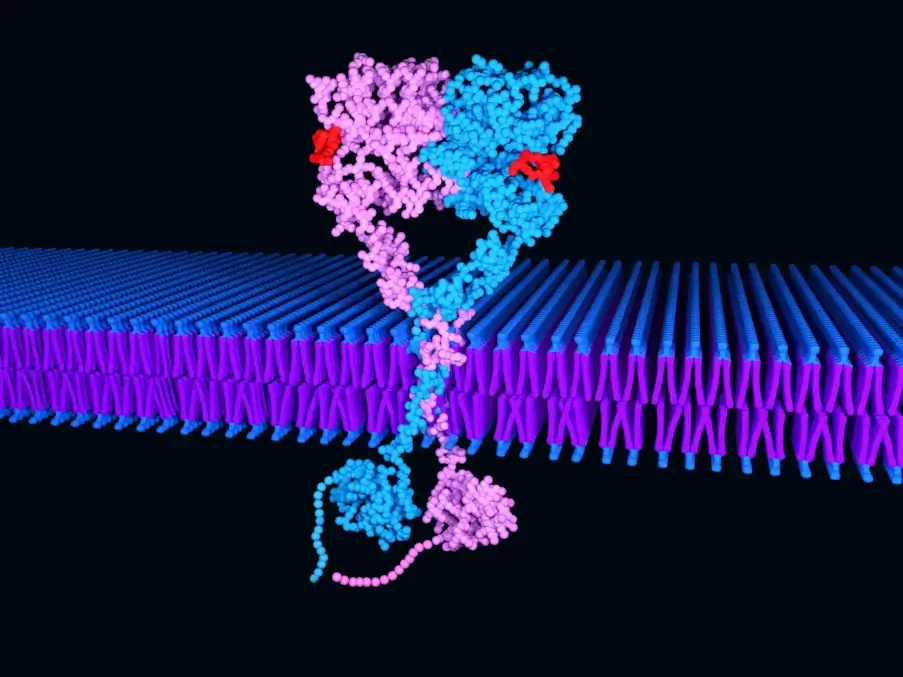
NSCLC is defined at the molecular level by key ‘driver’ alterations occurring in several genes, such as EGFR, KRAS, ALK, and FGFR. Approximately 10% of US NSCLC patients and 35% of patients in East Asia, have tumor-associated EGFR mutations within exons 18-21. Around 90% of EGFR mutations are exon 19 canonical in-frame deletions or exon 21 L858R point mutations, which confer increased sensitivity to first, second, and third generation EGFR tyrosine kinase inhibitors (TKIs).
The third most common EGFR mutation type is exon 20 insertions, which covers over 100 different variations of in-frame insertions and/or duplications and accounts for 4-10% of all EGFR mutant NSCLC. Unlike the more common exon 19/exon 21 mutations discussed above, exon 20 insertions result in decreased sensitivity to first and second EGFR TKIs, leaving a lack of treatment options for this patient class. Standard of care treatment for these patients is currently conventional cytotoxic therapies, similar to wild type EGFR tumors.
Developing More Relevant Preclinical NSCLC Models
Improved understanding and treatment options for these tumors are hindered by a lack of disease-relevant model systems, and the diverse nature and number of EGFR exon 20 insertions.
Floch et al used CRISPR technology and unique patient-derived translational xenograft models to assess the third generation EGFR TKI osimertinib and its metabolite (AZ5104) as a potential therapeutic option for this patient group.
Using CRISPR Gene Editing to Generate EGFR Exon 20 Insertion Cell Lines
First the researchers wanted to look at the activating potential and drug sensitivity of exon 20 insertions to EGFR TKIs. CRISPR gene editing was used to switch EGFR wild type alleles for the two most prevalent exon 20 insertions, D770_N771InsSVD and V769_D770InsASV, which cover 40% of patients with this mutation type. This provided clinically-relevant cell lines for downstream study.
In Vitro Efficacy Studies
These engineered cell lines were carried forward to in vitro studies, where osimertinib and AZ5104 potently inhibited phosphorylation, cell growth, and proliferation of the EGFR exon 20 insertion variants. Other first- and second-generation EGFR TKIs were assessed against these cell lines, and against cell lines with wild type EGFR, but osimertinib was shown to have a more favourable mutant-selective profile.
In Vivo Efficacy Testing with Cell Line Derived Xenograft Models
To test the in vivo efficacy of osimertinib against exon 20 insertions, the researchers used their CRISPR-generated cell lines to develop “conventional” cell line derived xenograft models. Afatinib was tested as a control and, as expected, both mutated xenografts were resistant to treatment representing a clinical afatinib dose.
By contrast, osimertinib induced significant tumor growth inhibition in both xenograft models, when compared with controls, and was also well-tolerated.
More Patient-Relevant In Vivo Efficacy Testing with PDX Models
While the in vitro and in vivo data presented in the paper was compelling, it was produced in non-endogenous engineered systems. Patient-derived xenograft (PDX) models provide a more patient-relevant preclinical model for assessing drug efficacy, as they are developed by directly implanting patient tumors in mice. Having never been manipulated to grow in vitro, these models more closely reflect patient tumors for histo- and molecular pathology and drug response.
Due to the rarity of exon 20 insertions in the clinical population, there is a lack of PDX models harboring these insertions. The study authors tested three models:
- LG1423 harboring V769_D770InsASV
- LXF2478 with M766_A767insASV mutation
- LU0387 carrying H773_V774insNPH mutation
For the LG1423 model, with the same mutation as the CRISPR-generated cell line, osimertinib treatment induced superior TGI than both afatinib and erlotinib. This was associated with inhibition of p-EGFR and downstream signalling markers.
The LXF2478 and LU3087 models, which carry less prevalent exon 20 insertions, were also sensitive to osimertinib and its metabolite, compared with control (and with afatinib for LXF2478). Combined, these data show that osimertinib is highly efficacious cross a number of patient-relevant exon 20 insertion models, potentially predicting efficacy in corresponding NSCLC patients with similar mutations.
Potential New Treatment Avenue for NSCLC Patients
Through CRISPR gene editing techniques, and use of the most predictive preclinical models, this new paper takes a comprehensive look at the use of osimertinib for use with NSCLC harboring EGFR exon 20 insertions. The authors suggest that the data provides enough evidence to start clinical testing of osimertinib for this patient class, where the drug could fill a great unmet need and provide the first targeted agent for this mutation type.